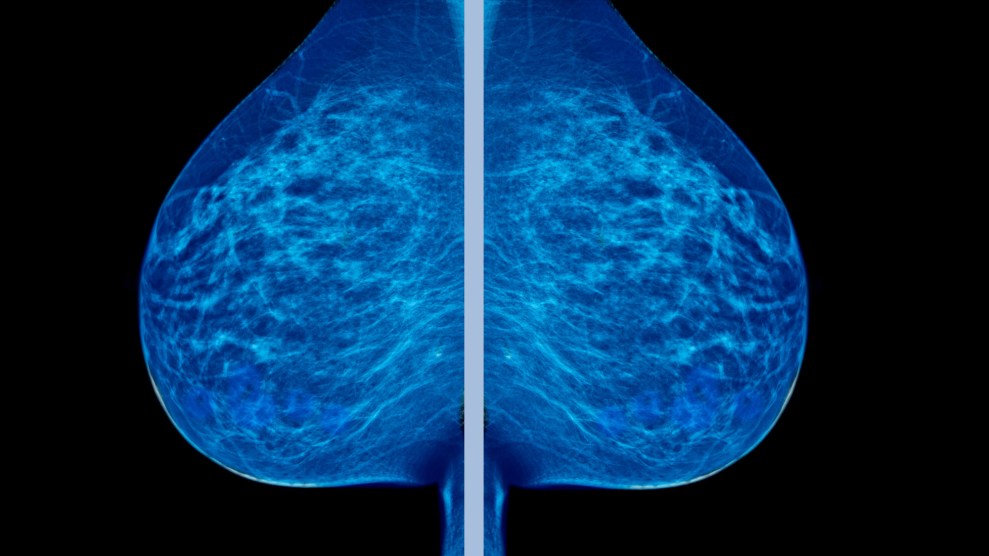
I thought I’d done everything right: breastfeeding my children, a careful diet, plenty of exercise. I wasn’t overweight and didn’t have a family history. I bought BPA-free bottles for my filtered water. But on a visit to the radiology department last spring, a pair of red brackets highlighted something worrisome on the ultrasound monitor.
Invasive lobular carcinoma—a malignant breast tumor. This spidery little beast measuring nearly three centimeters meant I had stage 2 cancer.
At 47, I was a decade and a half younger than the median age for breast cancer diagnosis in the United States. Was this just bad luck? Maybe, but the journalist in me was still curious to know: Why me? So I dug into the literature on risk factors to see where I might have fit in. It’s an impossible question to answer definitively for an individual, like trying to prove that a single weather event was caused by climate change. As one doctor told me, “You know who’s at risk for getting breast cancer? People with breasts!”
Still, most of the broad indicators didn’t seem to apply to me. The biggest one is age: The median diagnosis in the United States is at 62, and the highest breast cancer rates are in women older than 70. Another is taking hormone replacement therapy after menopause, but I’m premenopausal and haven’t taken it. Obesity raises risk, but I’ve never been overweight.
Then I saw one that gave me pause: alcohol consumption. I’m not a heavy drinker, but like most women I know, I have consumed a lot of alcohol in my lifetime.
While doctors have frequently admonished me for putting cream in my coffee lest it clog my arteries—a correlation that’s been pretty thoroughly debunked—not once has any doctor suggested I might face a higher cancer risk if I didn’t cut back on drinking. I’d filled out dozens of medical forms over the years asking how much I drank every week, but no one ever followed up other than to say with nodding approval, “So you drink socially.”
I quickly discovered that way back in 1988, the World Health Organization declared alcohol a Group 1 carcinogen, meaning that it’s been proved to cause cancer. There is no known safe dosage in humans, according to the WHO. Alcohol causes at least seven types of cancer, but it kills more women from breast cancer than from any other. The International Agency for Research on Cancer estimates that for every drink consumed daily, the risk of breast cancer goes up 7 percent.
The research linking alcohol to breast cancer is deadly solid. There’s no controversy here. Alcohol, regardless of whether it’s in Everclear or a vintage Bordeaux, is carcinogenic. More than 100 studies over several decades have reaffirmed the link with consistent results. The National Cancer Institute says alcohol raises breast cancer risk even at low levels.
I’m a pretty voracious reader of health news, and all of this came as a shock. I’d been told red wine was supposed to defend against heart disease, not give you cancer. And working at Mother Jones, I thought I’d written or read articles on everything that could maybe possibly cause cancer: sugar, plastic, milk, pesticides, shampoo, the wrong sunscreen, tap water…You name it, we’ve reported on the odds that it might give you cancer. As I schlepped back and forth to the hospital for surgery and radiation treatments, I started to wonder how I could know about the risk associated with all these other things but not alcohol. It turns out there was a good reason for my ignorance.
I was born and raised in Utah, and after my cancer diagnosis, I wondered what would have happened if I’d stayed put. My home state has one of the lowest rates of breast cancer in the country. Observant Mormon women don’t drink, and like other populations that abstain, they have significantly lower rates of breast cancer than drinkers. In Utah, Mormon women’s breast cancer rates are more than 24 percent lower than the national average. (Mormon men have lower rates of colon cancer, which alcohol can also cause.)
RELATED: What If Everything Your Doctors Told You About Breast Cancer Was Wrong?
Researchers suspect the low overall rate of breast cancer in Utah has to do with the LDS church’s strict control over state alcohol policy. Gentiles, as we non-Mormons are called, grouse mightily over the watery 3.2 percent beer sold in Utah supermarkets, the high price of vodka sold exclusively in state-run liquor stores, and the infamous “Zion Curtain,” a barrier that restaurants were until recently required to install to shield kids from seeing drinks poured. Yet all those restrictions on booze seem to make people in Utah healthier, Mormon or not, especially when it comes to breast cancer.
Epidemiologists first recognized the connection between cancer and alcohol consumption in the 1970s. Scientists have since found biological explanations for why alcohol is carcinogenic, particularly in breast tissue.
When you take a drink, enzymes in your mouth convert even small amounts of alcohol into high levels of acetaldehyde, a carcinogen. People who consume more than three drinks a day are two to three times likelier to contract oral cavity cancer than those who don’t. Alcohol also damages the cells in the mouth, priming the pump for other carcinogens: Studies have found that drinking and smoking together pose a much higher risk of throat, mouth, and esophageal cancer than either does on its own.
Alcohol continues its trail of cellular damage as enzymes from the esophagus to the colon convert it into acetaldehyde. The liver serves as the body’s detox center, but alcohol is toxic to liver cells and can scar the organ tissue, leading over time to cirrhosis, which raises the risk of liver cancer.
As acetaldehyde courses through the body, it can bind to DNA, causing mutations that can lead to cancer, particularly in the colon. Alcohol is suspected of inflicting a double whammy on breast tissue because it also increases the level of estrogen in a woman’s body. High levels of estrogen prompt faster cell division in the breast, which can lead to mutations and ultimately tumors.
Researchers estimate that alcohol accounts for 15 percent of US breast cancer cases and deaths—about 35,000 and 6,600 a year, respectively. That’s about three times more than the number of breast cancer cases caused by a mutation of the BRCA genes, which prompted Angelina Jolie, who carries one of the abnormal genes, to have both her healthy breasts removed in 2013. The breast cancer risk from alcohol isn’t nearly as high as the lung cancer risk from smoking. But alcohol-related breast cancer kills more than twice as many American women as drunk drivers do. And alcohol is one of the few breast cancer risk factors women can control. Others, like starting menstrual periods before the age of 12 and entering menopause after 55, are baked in.
Overall, American women have about a 12 percent lifetime risk of getting breast cancer. Walter Willett, an epidemiology professor at the Harvard T.H. Chan School of Public Health who has conducted studies on alcohol and breast cancer, says a woman who consumes two to three drinks a day has a lifetime risk of about 15 percent—a 25 percent increase over teetotalers. By comparison, mammography reduces the death rate from breast cancer by about 25 percent. “Alcohol can undo all of that at about two drinks a day,” Willett says.
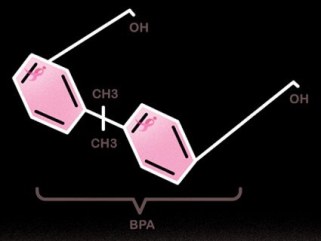
When the evidence of alcohol’s cancer risks emerged, public health advocates sought to spread the word. In 1988, California added alcohol to its list of cancer-causing chemicals that required a warning label. The next year, when Congress first mandated nationwide warning labels on alcohol, advocates tried to include cancer on them. Battered by activism around drunk driving and fetal alcohol syndrome, the booze industry was already in a slump, with alcohol consumption per capita on a steep slide since its 1981 peak. Fearing health advocates would do to alcohol what they had done to tobacco, the industry fought back with an audacious marketing campaign.
Alcohol companies worked to rebrand booze as a staple of a healthy lifestyle, like salads and jogging. The wine industry led, with vintner Robert Mondavi taking rabbis and doctors on educational tours about the alleged health benefits of moderate drinking. He told the New York Times in 1988 that wine “has been praised for centuries by rulers, philosophers, physicians, priests, and poets for life, health, and happiness.
The industry’s attempt to transform its products into health tonics might never have succeeded without the help of Morley Safer. In 1991, Safer hosted a 60 Minutes segment about the “French paradox,” the idea that the French eat heaps of red meat, cheese, and cream but have lower heart disease rates than Americans, who were many years into a low-fat dieting craze. On the show, he held up a glass of red wine and declared, “The answer to the riddle, the explanation of the paradox, may lie in this inviting glass.” New research, he said, showed red wine might flush out fatty deposits on artery walls and counteract the effects of the heavy French diet.
That TV episode, which according to the International Wine & Food Society was viewed by more than 20 million people, created a media sensation and caused a spike in red wine sales nationwide. Researchers soon debunked the idea that wine was helping French heart health, and France’s heart disease rate turned out to be higher than advertised. Meanwhile, all the wine the French consumed was killing large numbers of them. The same year as the 60 Minutes episode, France passed some of the world’s strictest regulations of alcohol advertising to combat prevalent liver cirrhosis.
Even so, the US wine industry lobbied to include a positive health message about alcohol in the 1995 Dietary Guidelines for Americans published by the Department of Agriculture. The new guidelines removed language indicating that alcohol had “no net health benefit” and stated that for some people, moderate alcohol consumption might reduce the risk of heart disease.
At a conference of beer wholesalers in 1996, the Miller Brewing Co.’s vice president of corporate relations touted the success of the 60 Minutes episode and the subsequent changes in government health messages as progress in the industry’s effort to brand its products as healthy. She urged attendees to open every meeting with an elected official by saying, “Alcohol can be part of a healthy diet.”
Over the past two decades, the alcohol industry has gone all out to tie its products to an active lifestyle. Peter Cressy, the former CEO of the Distilled Spirits Council of the United States (DISCUS), the liquor lobby, explained in 2000, “DISCUS is working to ensure cultural acceptance of alcohol beverages by ‘normalizing’ them in the minds of consumers as a healthy part of a normal lifestyle.”
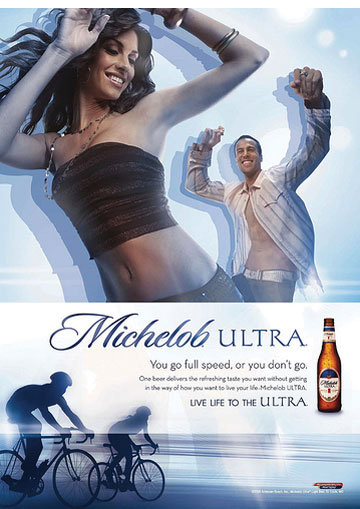
Alcohol companies, long sponsors of football games and NASCAR events, now sponsor 5K races and triathlons. During last year’s Super Bowl, a Michelob Ultra ad featured extremely fit people working out and then grabbing a beer to quench their thirst. (Drinking alcohol after exercise causes dehydration and impedes muscle recovery.) Hard liquor companies concocted products like Devotion Spirits vodka, which supposedly contained a protein that would help build muscle while preventing hangovers. (In 2012, Devotion Spirits withdrew many of its health claims after the Federal Trade Commission opened an investigation.)
Indeed, the supposed health upside of moderate drinking is one of the industry’s go-to talking points. When Mother Jones reached out to the leading beer and liquor companies and the major industry groups, those that responded acknowledged the connection between alcohol and cancer, but some argued the risk belongs mostly or entirely to heavy drinkers. Sarah Longwell, the managing director of the American Beverage Institute, said in a statement that “a substantial number of well-conducted studies reveal no correlation between cancer and moderate to light alcohol consumption.” Moderate drinking, she noted, has been found to reduce the risk of heart disease, among other benefits. “There has been a concerted effort by some researchers to reverse that knowledge,” she said in an earlier conversation. “I think it is flying in the face of good science.”

Marketing alcohol as a health product should be a tough sell. Cancer is only one of the many ways it can kill you. Drunk driving, alcohol poisoning, injuries, domestic violence, liver disease—alcohol is responsible for the deaths of nearly 90,000 Americans every year, more than double the estimated 40,000 US opioid deaths in 2015. To overcome this hurdle, the industry needed to give its PR campaign scientific backing. The strategy came straight from the tobacco playbook, which wasn’t a surprise: Sometimes the companies were one and the same. The tobacco giant Philip Morris, which bought Miller in 1970, later became Altria, which today has a big stake in Anheuser-Busch.
Big Tobacco had set up research centers to dispute science tying smoking to lung cancer and funded research designed to show benefits from smoking, like stress reduction, to help fend off stricter regulation. The alcohol industry took a similar tack, aided by research it had been funding since the late 1960s. In a 1993 book called Forward Together: Industry and Academia, Thomas Turner, the former dean of the Johns Hopkins University medical school, explained how, starting in 1969, he had worked with the heads of the world’s biggest beer companies to create the Alcoholic Beverage Medical Research Foundation (now called the Foundation for Alcohol Research). The foundation took academics to exotic destinations for conferences and gave grants to scientists.
Between 1972 and 1993, Turner bragged, the beer foundation and its precursor funded more than 500 studies on alcohol and distributed grants to dozens of researchers and universities. One was Dr. Arthur Klatsky of Kaiser Permanente. In the early 1970s, Klatsky had access to extensive data through Kaiser’s health system that included information about patients’ alcohol intake. In 1974, he published one of the first papers suggesting that light drinkers had lower rates of heart disease than abstainers. Soon after, the beer foundation started funding Klatsky’s data collection at Kaiser, a relationship that continued for decades. Between 1975 and 1991, according to Turner’s book, the foundation contributed $1.7 million to Klatsky’s research on alcohol and health. The industry widely promoted his work suggesting health benefits from drinking, and Klatsky is still quoted regularly in the media, often without any disclosure of his relationship with the industry.
Klatsky says industry funding has never compromised the objectivity of his research. He notes that the first study he did with beer foundation money showed that drinkers had an elevated risk of high blood pressure. He also published an early study on the link between alcohol and breast cancer. “I think that most people who know me and know my work think I’m unbiased,” he told me. “I see both sides of the alcohol issue. It’s a double-edged sword.”
The industry has also funded researchers who cast doubt on studies that pose problems for it. For example, the Distilled Spirits Council paid for a 1994 study by Dr. H. Daniel Roth, who was then helping Philip Morris reach a settlement with lung cancer victims, that disputed the link between alcohol and breast cancer. “You’re looking at industries that are adept at creating doubt when it comes to protecting their profits,” says Robert S. Pezzolesi, the founding director of the public health group New York Alcohol Policy Alliance.
In the early 1990s, the beer foundation funded research by George Koob, who served as a foundation adviser between 1999 and 2003. In 2014, he became director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the only federal agency devoted exclusively to alcohol research.
Washington’s revolving door sends people in both directions. At least a half-dozen government officials working on alcohol policy have left for gigs with the industry over the past 20 years. Among the most prominent is Dr. Samir Zakhari, the former director of the Division of Metabolism and Health Effects at the NIAAA. In 2012, the Distilled Spirits Council hired him to head its science office.
RELATED: Is Susan G. Komen Denying the BPA-Breast Cancer Link?
The NIAAA has long recognized that alcohol increases breast cancer risk, and literature on the Distilled Spirits Council’s website acknowledged this, too, although it appears to have been taken down. But in 2015, Zakhari published a scientific journal article asserting that “there is no solid evidence associating moderate alcohol consumption with an increased incidence of breast cancer.” He advised women worried about cancer to consult a doctor because “moderate alcohol consumption has been associated with potential health benefits, including decreased risk of coronary artery disease and overall mortality, protection against congestive heart failure, decreased risk of ischemic stroke, and protection against type 2 diabetes and rheumatoid arthritis.” An industry group recently cited the paper to try to fend off restrictive government recommendations about alcohol consumption in the United Kingdom.
Zakhari keeps in touch with his old colleagues at the NIAAA, according to emails Mother Jones obtained through a public records request. In 2014, the Baltimore Sun ran an op-ed by the industry-supported Competitive Enterprise Institute that complained tax dollars were paying for “anti-alcohol advocacy” and cited an NIAAA-funded study about industry marketing to underage drinkers that had been conducted by David Jernigan, the director of the Johns Hopkins University Center on Alcohol Marketing and Youth. An email circulated among NIAAA employees alerting them to the article. Koob, the NIAAA director, forwarded the email thread to Zakhari and wrote, “Sam: For the record. This will NOT happen again. I will NOT be funding this kind of work under my tenure.” Zakhari responded that some researchers advocated these types of studies “out of shear [sic] ignorance or because they are sympathetic,” but that he was confident Koob would “spend research money on real science.”
Zakhari takes issue with the idea that he is emblematic of Washington’s revolving door and says the 2015 paper “reflects my personal scientific opinion.” In a statement to Mother Jones, he said, “I came to the Council, after my retirement from NIH, because I share their commitment to responsible alcohol consumption. My dedication to evidence-based research remains the same regardless of where I am employed.”
My discovery that alcohol consumption was a risk factor for my breast cancer contradicted everything I thought I knew about drinking. Like 76 percent of Americans surveyed by the American Heart Association in 2011, I believed a little wine was good for the ticker. The fact is, people want to believe that drinking is good for them, and the science in this field is easy to manipulate to convince them.
Scientists have long known that heavy drinking causes high blood pressure, strokes, and heart attacks. That’s why early studies investigating drinking and heart disease started with the logical supposition that people who abstain from alcohol should have low rates of heart disease compared with moderate or heavy drinkers. As it turned out, they didn’t. When plotted on a curve, drinkers fell into a J-shaped pattern: Abstainers in the studies had rates of cardiovascular disease similar to those of heavy drinkers.
But this J-curve is deceptive. Not all the nondrinkers in these studies were teetotalers like the ones I grew up with in Utah. The British epidemiologist A. Gerald Shaper began a wide-ranging men’s heart health study in the late 1970s, and when he examined the data, he found that 71 percent of nondrinkers in the study were actually former drinkers who had quit. Some of these ex-drinking men were as likely to smoke as heavy drinkers. They had the highest rate of heart disease of any group and elevated rates of high blood pressure, peptic ulcers, diabetes, gallbladder disease, and even bronchitis. Shaper concluded that ex-drinkers were often sicker than heavy drinkers who hadn’t quit, making them a poor control group.
Yet for decades, researchers continued to include them and consequently found an implausible number of health benefits to moderate drinking, including lower rates of deafness and liver cirrhosis. The industry has helped promote these studies to doctors.
That’s one reason why, until recently, alcohol’s heart health benefits have been treated as incontrovertible science. But in the mid-2000s, Kaye Middleton Fillmore, a researcher at the University of California-San Francisco, decided to study Shaper’s ex-drinkers. When no one in the United States would fund her work, she persuaded Tim Stockwell, then the director of Australia’s National Drug Research Institute, to help her secure Australian government funding.
Stockwell and Fillmore analyzed decades’ worth of studies on alcohol and heart disease. Once they excluded studies with ex-drinkers—which was most of them—the heart benefits of alcohol largely disappeared. Since then, a host of other studies have found that drinking does not provide any heart benefits. (Some studies have found that drinking small amounts of alcohol—sometimes less than one drink per day—can be beneficial for certain people at risk of heart disease.) Robert Brewer, who runs an alcohol program at the Centers for Disease Control and Prevention, says, “Studies do not support that there are benefits of moderate drinking.” The Agriculture Department removed language suggesting that alcohol may lower the risk of heart disease in the most recent US Dietary Guidelines.
Yet the debate rages on, in part because the industry continues to fund and promote studies indicating that alcohol helps the heart. The NIAAA is currently embarking on another one with $100 million in funding, most of which was solicited directly from the industry, according to the New York Times. The study was planned in consultation with industry leaders and pitched as a way to prove that moderate drinking can be healthy. It is being billed as the most definitive study on moderate drinking to date, but it will likely understate the risks, partly because it won’t run long enough to track any increases in cancer rates. At least five researchers on the project are past recipients of industry money.
Public health experts say that even if there is a small heart benefit from alcohol, it will never outweigh the risks. Alcohol “would never be approved as a medicine,” says Jennie Connor, a preventive- and social-medicine professor at the University of Otago in New Zealand who wrote one of the landmark papers linking alcohol to cancer. “It’s addictive, like opioids. If you give medication to people that could affect their unborn child or make them aggressive and hit their wife, what kind of medicine is that? From a public health standpoint, using alcohol for heart disease is utterly wrong. It goes against everything medical people do.”
“From a pure scientific perspective, what is the point of this [pro-alcohol] research?” asks Michael Siegel, a professor at the Boston University School of Public Health. “How is it going to change policy or practice? It’s not. Even if it turns out that there are true benefits, we’re not going to start recommending that people who have never had alcohol before start drinking.”
There are far safer ways than drinking to reduce the risk of heart disease—walking, for instance—that also won’t give you cancer. That’s why the American Heart Association strongly warns people not to start drinking if they don’t already.
I drank my first beer when I was 13. My dad and I had been out pheasant hunting on a cold day. After we bagged our birds, we got into the Jeep to warm up, and my dad handed me a Mickey’s Big Mouth. It was nasty, but I drank it to prove my worthiness of the adult gesture. When I was done, he said, “You wanna drive?” That was Utah in the ’80s, at least if you weren’t Mormon.
Later, I went to a Catholic high school, where we distinguished ourselves from the future missionaries in the public schools with excessive drinking. Even in Utah, booze was easy to come by. There was Doug at Metro Mart, who sold us beer from the drive-thru window. When he wasn’t around, we stole it from our parents, siphoning off small amounts of bourbon, rum, gin, and vodka and then dumping the whole awful mix into a cola-flavored Slurpee and sucking it down through a straw.
I went off to the University of Oregon, where Animal House had been filmed 10 years earlier. During my time there, the university decided to crack down on underage drinking on campus. Riots broke out, and the local police had to deploy tear gas.
I’ve never drunk as heavily as I did before I could legally buy a drink. My experience isn’t unusual. Ninety percent of alcohol consumption by underage Americans is binge drinking, defined as four or more drinks on one occasion, according to the CDC. I’ll never know for sure, but all the drinking I did in my adolescence may have helped pave the way for the cancer I got at 47.
Human breast tissue doesn’t fully mature until a woman becomes pregnant. Before then, and particularly during puberty, breast cells proliferate rapidly, which may make them especially vulnerable to carcinogens. That’s one reason why never getting pregnant is itself a risk factor for breast cancer. Scientists have understood this for nearly 40 years, thanks to studies of women in Nagasaki exposed to radiation from the atomic bomb. Japanese women who’d been exposed before age 20 had the highest rates of breast cancer. Other studies suggest that the risk of premenopausal breast cancer goes up 34 percent for every daily drink consumed before the age of 30. And the longer women go between their first period and their first baby, the riskier drinking becomes.
With a first pregnancy at 33, I had a good 20 years of drinking to damage my breasts, and my adolescent binge drinking may have been especially devastating. Dr. Graham Colditz, a cancer prevention specialist and epidemiologist at Washington University in St. Louis, wrote in the British medical journal Women’s Health in 2015 that “women who report seven drinks on the weekend but no alcohol consumption on the weekdays may have higher risk of breast cancer as compared with those who consistently have one drink every day.” One study Colditz cited found a nearly 50 percent increase in breast cancer risk among women who consumed 10 to 15 drinks over a typical weekend compared with those who had no more than three.
Colditz says cancer prevention efforts haven’t kept up with demographic trends. As women across the globe have delayed childbearing, he says, “We’ve really extended this period of life when the breast is most susceptible, and we haven’t mounted a prevention strategy to counter the marketing of alcohol.”
Liquored Up
US per-capita alcohol consumption, in gallons of ethanol per year
Source: National Institute on Alcohol Abuse and Alcoholism
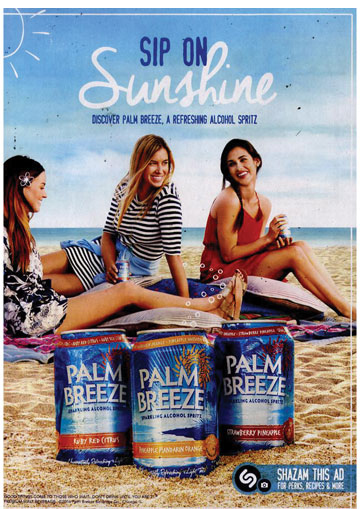
In fact, just as the evidence was becoming clear that women are disproportionately vulnerable to alcohol’s cancer risks, the industry mounted a campaign to get them to drink even more. “Women all over the world are underperforming consumers,” explains Jernigan, the Johns Hopkins researcher who is now a professor at the Boston University School of Public Health. The distilled spirits industry, facing flagging sales, created “alcopops”—sweetened alcoholic beverages such as Zima, Smirnoff Ice, and Skyy Blue that are packaged in childlike bright colors. Marlene Coulis, director of new products at Anheuser-Busch, explained in 2002, “The beauty of this category is that it brings in new drinkers, people who really don’t like the taste of beer.”
Just who were those “new drinkers” who didn’t like beer? Federal data shows the median age for the first consumption of alcohol is about 14, and Jernigan says the people who don’t like the taste of beer tend to be young women. The alcopop-makers managed to convince state and federal regulators that the products were “flavored malt beverages” like beer, even though the main ingredient was distilled spirits. The designation allowed companies to sell these products in convenience stores that also sold beer, at a much lower tax rate than hard liquor required, making them more accessible to underage drinkers. The liquor companies then blasted the youth market with ads for the new products.
The distilled spirits industry had voluntarily given up advertising on the radio back in 1936 and on TV in 1948 to avoid regulation by Congress, but it jettisoned those pledges in 1996. Still, TV liquor ads didn’t fully take off until the advent of alcopops. In 2001, says Jernigan, there were fewer than 2,000 ads for spirits on cable TV. In 2009, that figure had jumped to more than 60,000, and many ads targeted TV audiences with large numbers of viewers too young to drink legally. (In 2012, all the major TV broadcast networks also abandoned their ban on liquor ads.) In an email to Mother Jones, Coulis said the idea that alcopops were intended to appeal to underage drinkers is a “gross mischaracterization and absolute falsehood.”
Traditionally, young people in the United States have been beer drinkers, but in the early 2000s, surveys showed that women were increasingly turning to harder stuff, and they’ve remained there. Ads and products now push alcohol as a salve for the highly stressed American woman. There are wines called Mother’s Little Helper, Happy Bitch, Mad Housewife, and Relax. Her Spirit vodka comes with swag emblazoned with girl-power slogans like “Drink responsibly. Dream recklessly.” Johnnie Walker recently came out with Jane Walker scotch, to market a liquor “seen as particularly intimidating by women,” according to the company. (Johnnie Walker is owned by Diageo, a multinational alcohol conglomerate. One of Mother Jones‘ board members is also an executive at Diageo.)
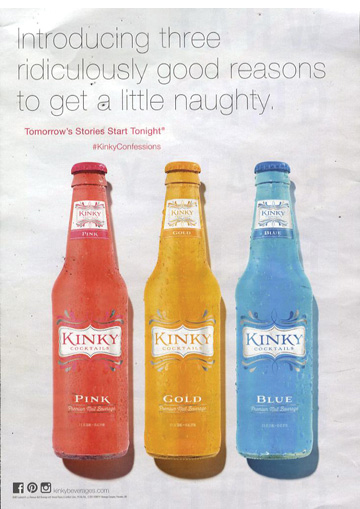
Booze-makers have also “pinkwashed” products targeted at women, literally draping the ads in pink ribbons, with promises to donate some proceeds to breast cancer charities. In 2015, Alcohol Justice, a California-based policy advocacy group, found 17 brands of pinkwashed booze. “They’re marketing a carcinogen,” says the New York Alcohol Policy Alliance’s Pezzolesi. “Can you imagine if Philip Morris did a pink tobacco pack? People would be up in arms.”
The campaigns seem to have worked. An NIAAA study found that drinking by women jumped 16 percent between 2001 and 2013, more than twice the increase among men. The change is greatest among white women, 71 percent of whom drink today, compared with 64 percent in 1997, according to a Washington Post analysis. The alcohol-related death rate for white women more than doubled between 1999 and 2015.
The ad is graphic: A glass of red wine spills onto a white tablecloth and starts to form the image of a woman. “Alcohol is carcinogenic,” the narrator says. “Once absorbed into the bloodstream, it travels through the body. With every drink, the risk of cell mutations in the breast, liver, bowel, and throat increases. These cell mutations are also known as cancer.” The wine pools around the woman like blood, and the narrator advises limiting cancer risk by not having more than two drinks on any day. The ad campaign aired in 2010 in Western Australia.
In England in 2013, a public health charity broadcast an ad campaign featuring a man drinking a beer with a tumor at the bottom of the glass, which he ultimately swallows as the narrator explains, “The World Health Organization classifies alcohol as a Group 1 carcinogen. Like tobacco and asbestos, it can cause cancer.”
Other countries have begun to take heed of alcohol’s cancer risks. For the first time, in 2010, the World Health Organization issued a global strategy for reducing the harms of alcohol. It recognized cancer as one of those harms and called on countries to implement measures to lower consumption. Many have done so. South Korea has tightened its recommended alcohol limits, and new Dutch guidelines urge people not to drink at all, but if they do, to consume no more than one drink a day. In December, Ireland’s upper house of parliament approved a cancer warning label for alcohol that is now being debated in the lower house. Even the Russians raised their alcohol taxes. (Canada recently launched an experiment to test cancer warning labels on alcohol in the Yukon but stopped the project a month later amid intense pressure from alcohol companies.)
In 2016, Britain reduced its recommended alcohol consumption limit for men to the same level as for women, about six pints of beer a week. Sally Davies, the chief medical officer for England, told the BBC, “If you take 1,000 women, 110 will get breast cancer without drinking. Drink up to these guidelines and an extra 20 women will get cancer because of that drinking. Double the guideline limit and an extra 50 women per 1,000 will get cancer…That’s not scaremongering. That’s fact.”
It’s not the kind of straight talk you’re likely to hear in the United States, where the industry is fighting to prevent cancer fears from hurting its bottom line. In spring 2016, the American Beverage Institute’s Longwell told a brewers’ conference that public health officials “want to tell you that alcohol causes cancer,” according to the Wall Street Journal. Such public health activism, she suggested, was a threat to the industry’s “health halo.” At another 2016 conference, Jim McGreevy, president of the Beer Institute, an industry lobbying group, said of public health advocates, “We can’t let them gain traction.” He did not respond to a request for comment.
Pinkwashing
Alcohol companies have tried to persuade consumers they can help fight breast cancer by purchasing “pinkwashed” products that benefit cancer charities, obscuring alcohol’s proven breast cancer risk.


For more than a decade, the alcohol industry has bulldozed long-standing public health regulations designed to reduce harmful consumption. It has mounted successful campaigns to allow the sale of liquor in supermarkets and on Sundays and to loosen restrictions on the hours liquor can be served in restaurants and bars. Not surprisingly, alcohol consumption per capita in the United States, which hit a 34-year low in 1997, has shot up to levels not seen in two decades.
Alcohol companies are enormous multinational corporations. AB InBev controls nearly 50 percent of the US beer market, including the all-American brand Budweiser. Jernigan analyzed Nielsen data and estimated that the industry spent $2.1 billion on advertising in 2016, a figure that doesn’t include online ads or those in stores. It also spent $30.5 million last year to lobby Congress. The Distilled Spirits Council, which alone spent $5.6 million on federal lobbying last year, holds whiskey tastings on Capitol Hill attended by Democrats and Republicans alike. “Alcohol is the drug of choice of the people who make the laws,” observes Jernigan.
While other countries are considering World Health Organization recommendations to impose steeper alcohol taxes, the tax law President Donald Trump signed in December further slashed US alcohol excise taxes, which, thanks to inflation, were already down as much as 80 percent since the 1950s.
Under the Influence
Alcohol industry spending on lobbying
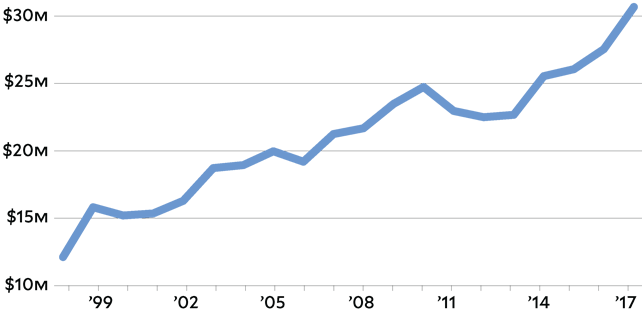
Source: OpenSecrets
Koob, the NIAAA director, has attended events at the Distilled Spirits Council and met with its representatives, according to documents obtained through a public records request. He gets holiday party invites from the Beer Institute and meets with its CEO. In 2015, Koob and the NIAAA’s director of global alcohol research appeared in a promotional video for AB InBev’s “global smart drinking goals,” filmed at an AB InBev Global Advisory Council meeting.
“We went through the normal procedures here at NIH for approval, and we were given approval to do it,” says Koob. “Under no circumstances are we promoting alcohol beverages or any product. That’s not our nature. But if people want to help prevent alcohol misuse, we’re all for it.”
Boston University’s Siegel counters, “The whole idea [behind the campaign] is that if you drink properly, not to excess, it’s okay. That’s not true. If you drink moderately, you’re increasing your risk of cancer, and that’s the part of it they don’t want people to know.”
After I had surgery to remove my tumor, my oncologist sent me to see the cancer dietitian last June. The dietitian outlined a joyless regimen so complex it required a spreadsheet for compliance. Along with more fish and flaxseed, she recommended five weekly servings of cruciferous vegetables like broccoli, as well as loads of beans for additional fiber. She put the kibosh on bacon and sausage—processed meats are considered carcinogenic. She instructed me to eat natural soy like tofu at least three times a week but not processed soy like that found in garden burgers because it can boost cancer-causing estrogen levels. And she sternly admonished me to lay off the cream in my coffee.
Not once did the subject of alcohol come up. “There’s more data for counseling you to decrease alcohol than to eat broccoli or tofu,” says Noelle K. LoConte, an oncologist and associate professor at the University of Wisconsin. But she says the message about alcohol and cancer hasn’t gotten out, even to cancer doctors, which may be one reason not a single one of my doctors raised the issue with me before or after I was diagnosed.
To address this problem, in November LoConte co-authored a statement from the American Society of Clinical Oncology that officially declared alcohol a cancer risk. (The society also commissioned a poll, which found that 70 percent of Americans had no idea alcohol can cause cancer.) In its statement, the group called for policy measures to reduce alcohol consumption and prevent cancer, the same ones recommended by the US surgeon general, the federal Community Preventive Health Task Force, and the World Health Organization. They’re similar to strategies that brought down smoking rates: higher excise taxes, limits on the number of outlets selling alcohol in a particular area, stricter enforcement of underage drinking laws, and caps on the numbers of days and hours when alcohol can be sold.
There’s a huge body of research supporting the effectiveness of these policies, yet there is not a single public health group in Washington lobbying for any of them. The few groups that once battled with the alcohol industry have abandoned the effort in recent years. The American Medical Association, which used to focus on alcohol-related harm and campus binge drinking, stopped working on alcohol policy in 2005. The Ralph Nader-linked Center for Science in the Public Interest stopped during a budget crunch in 2009. That same year, the Robert Wood Johnson Foundation, which for decades had been one of the biggest funders of efforts to reduce underage drinking, largely pulled out of the field.
“It’s astounding that one of the leading causes of premature death and illness is ignored by almost every foundation that works in the health area,” says Richard Yoast, who ran the AMA’s alcohol programs until they ended in 2005.
Pop Culture
In the early 2000s, the alcohol industry sought to attract new drinkers—often young and female—with “alcopops,” sweetened drinks in bright childlike colors. The industry has also tried to brand alcohol as healthy with ads featuring athletes.
Government funding for alcohol harm reduction has also dried up. In 2009, the Justice Department budget for grants to states to enforce underage drinking laws was $25 million. By 2015, it was zero. At the request of the Obama White House, Congress also eliminated an Education Department program that combated underage drinking, among other initiatives.
Without independent funding for public health work on alcohol policy, the industry has filled the void, creating nonprofits to promote “responsible” drinking. Industry groups have used these to respond to the news about alcohol and cancer. When I asked the Beer Institute to comment for this story, a spokesman sent me a link to a report from the International Alliance for Responsible Drinking, a nonprofit funded by the world’s largest alcohol companies, and quoted one line from the report: “The most clear association of cancer risk is with heavy drinking, particularly regular heavy drinking over extended periods of time.”
Mark Petticrew, a professor of public health at the London School of Hygiene and Tropical Medicine, recently published a study finding that many alcohol industry websites and nonprofits have actively misled the public about the link between alcohol and cancer. They suggest that only problem drinkers have an elevated risk of cancer and present long lists of other risk factors to confuse readers, particularly when it comes to breast cancer. “Female consumers are more health conscious than male consumers,” Petticrew explains. “The female consumer is seen as part of the alcohol market that needs to be marketed to more. The female drinker is the last person you want to be a fully informed consumer.”
Over the past 30 years, breast cancer survivors have become a powerful political force in their own right, raising millions of dollars for research and education. But wine tastings are a staple of breast cancer fundraising events. The Lombardi Comprehensive Cancer Center at Georgetown University has been holding a “women and wine” fundraiser annually for breast cancer research for more than a decade. “Brews for Breast Cancer” events have proliferated. In October, the American Cancer Society threw its 40th annual Wine and Spirits Industry Gala in New York City “to support the Society’s mission of eliminating cancer as a major health problem.”
In response to questions from Mother Jones, Dr. Richard Wender, the chief cancer control officer for the American Cancer Society, says alcohol is much less risky than tobacco. “Our goal is to find the right balance that allows companies to engage with us, while staying true to our values and our public health mission,” he says.
The more I looked into the conflicts of interest among those responsible for informing the public of alcohol’s health risks, the more I began to recognize my own industry’s entanglement. The press, which starting with Morley Safer has flooded readers with stories declaring that drinking is good for your health, has repeatedly accepted alcohol companies’ largesse. In 2016, the Wall Street Journal sponsored a party with the Distilled Spirits Council at the Republican National Convention. In April 2017, the council and the Beer Institute helped pay for a “Toast to the First Amendment” party with RealClearPolitics.
In 2016, the president of the Distilled Spirits Council, Kraig Naasz, wrote in an email newsletter that the group had recently treated writers from a wide range of publications to cocktails at a New York bar during a lunch briefing on alcohol and health. On hand to chat up the journalists was Zakhari, the former NIAAA scientist. “The presenters underscored that moderate alcohol consumption can be incorporated into a healthy adult diet,” Naasz reported.
The Foundation for Advancing Alcohol Responsibility, funded by companies such as Bacardi and Diageo, paid for journalists to attend workshops last year held by the Poynter Institute, the self-appointed watchdog of journalism ethics. “The conflict of interest is so big it makes me gasp,” New York University nutritionist Marion Nestle told Health News Review when it broke the story on Poynter. “The alcohol industry wants journalists to extol the (purported) health benefits of drinking alcohol and to minimize the risks.”
Kelly McBride, Poynter’s vice president, says the foundation’s involvement did not affect the content of the workshops and the institute may collaborate with the foundation again. “They are a non-profit foundation that promotes responsible consumption of alcohol,” she said in an email. “They funded workshops where we taught journalists to apply the skills of fact-checking to scientific research. That seems like a consistent overlap of purpose.”
Susan Sontag once wrote that telling people about your cancer diagnosis tends to fill them with mortal dread. But when I’ve disclosed my illness to friends and told them that alcohol can cause breast cancer, I’ve never invoked enough mortal dread to deter anyone from ordering a second drink. Most women have no idea drinking causes breast cancer, and they really don’t want to be told that it does.
Marisa Weiss, a breast oncologist and the founder of BreastCancer.org, gives talks on college campuses, where she explains to young women the cancer risks they face from drinking. “I see the same people get completely trashed that night,” she laments. But she understands why. “It’s because life is a bitch,” she says. “We work long hours, and alcohol becomes like self-medication. It’s relaxing. It’s fun.”
I get it. But you know what’s not fun? Watching your 10-year-old daughter keen and hyperventilate after you tell her you have cancer. Or having six-inch needles full of radioactive dye plunged repeatedly through your nipple, without anesthesia, so a surgeon can see if the cancer has spread to your lymph nodes. Or leaving work early while awaiting biopsy results because your hands are shaking so badly you can’t type. Cancer isn’t fun, in ways far beyond the obvious. And in relative terms, I’ve had it easy so far. I’m still alive.
A few months ago, I plugged my data into the National Cancer Institute’s breast cancer risk calculator to see what my odds had been before I discovered my tumor. The bare-bones assessment showed I had a 1.1 percent risk of getting breast cancer in the next five years. The calculator doesn’t account for my alcohol consumption (or the protective effects of exercise and breastfeeding), but the experts I’ve spoken with say booze probably bumped up my risk.
I’ll never know for certain whether alcohol caused my cancer. There are so many factors: Just in December, a Danish study found that being on birth control raises the risk of breast cancer more than previously thought. What I do know is that cutting back on drinking, particularly when I was young, is virtually the only thing I could have changed about my lifestyle to try to prevent this cancer if I’d been fully informed. Now I’ve mostly given up alcohol to hedge my bets against a recurrence. I can’t be sure I would have done the same thing if someone had told me when I was 15 or 20 that drinking could give me breast cancer. I’d like to think so—I never smoked—but there’s no guarantee I wouldn’t have been just like the students Weiss talks to. At least they have a choice—they’ve been told the risk they’re taking. Like most women, I didn’t have that choice, and a powerful industry worked to keep it that way.
So, what do you think?
Tell us how you’re reacting to this story by sharing your thoughts. We may use your response in a follow up story.
We may share your response with our staff and publish a selection of stories which could include your name, age, and location. We respect your privacy. Your email address will not be published and by providing it, you agree to let us contact you regarding your response.