Meredith Legg Stapleton was was taking a shower one day when suddenly her left eye went dark, like a curtain falling. It was just a few months before her graduation from the University of South Carolina, Aiken, and Meredith, as a basketball star from Huntersville, North Carolina, knew that retinas could tear and thought hers might have. She was known as Mighty Warrior and Heaven’s Warrior, references to her athletic prowess and devout religious faith. She was on a scholarship and had the single-season record for consecutive free throws and her university’s all-time scoring record. But what happened in the shower threw her entire future into flux.
It was a point of no return—she’d never regain sight in that eye. A visit to a local ophthalmologist on a Friday afternoon revealed a large tumor he suspected was ocular melanoma (OM). Meredith and her family then drove 13 hours that weekend to one of the leading OM treatment centers in the country: Wills Eye Hospital, which is part of Thomas Jefferson University Hospital in Philadelphia. Oncologists confirmed the suspected diagnosis. The optimal treatment? Remove her eye.
OM is an extremely rare and aggressive form of cancer; there are only about 2,500 cases each year in the United States. Doctors call it “uveal melanoma,” named after the uvea, a structure of the eye that contains the iris, the ciliary body that surrounds it, and the choroid, a vascular layer between the white of the eye and the retina. Melanoma cancers can start in any of these tissues, but the most dangerous and difficult to treat are in the ciliary body and choroid because tumors can grow invisibly there for years before detection. That’s where Meredith’s cancer appeared. Confined to the eye, OM doesn’t kill. But half the time, the cancer spreads to the liver and, once it does, 80 percent of the cases are fatal within seven years, although the mortality rates vary. Some patients only survive five to 12 months after metastases; others have survived decades.
When Meredith heard the doctor’s recommendation, she announced that she had no intention of following orders, insisting she wanted them “to do everything to save my eye.” Meredith’s mother, Robin Legg, says, “She was a take charge personality. She even read her own chart while awaiting her eye specialist.” After further tests, the oncologist recommended radiation plaque therapy, a procedure that uses rice-size radioactive seeds contained within a gold or steel bowl (called a “plaque”) that’s surgically implanted inside the eye socket for a week to deliver targeted radiation. Meredith slept 20 hours a day and described the pain as “sticking an ice pick in the eye.” A month later, wearing a patch over her left eye, she graduated cum laude with the class of 2009 and continued to work, volunteer coach, and play basketball.
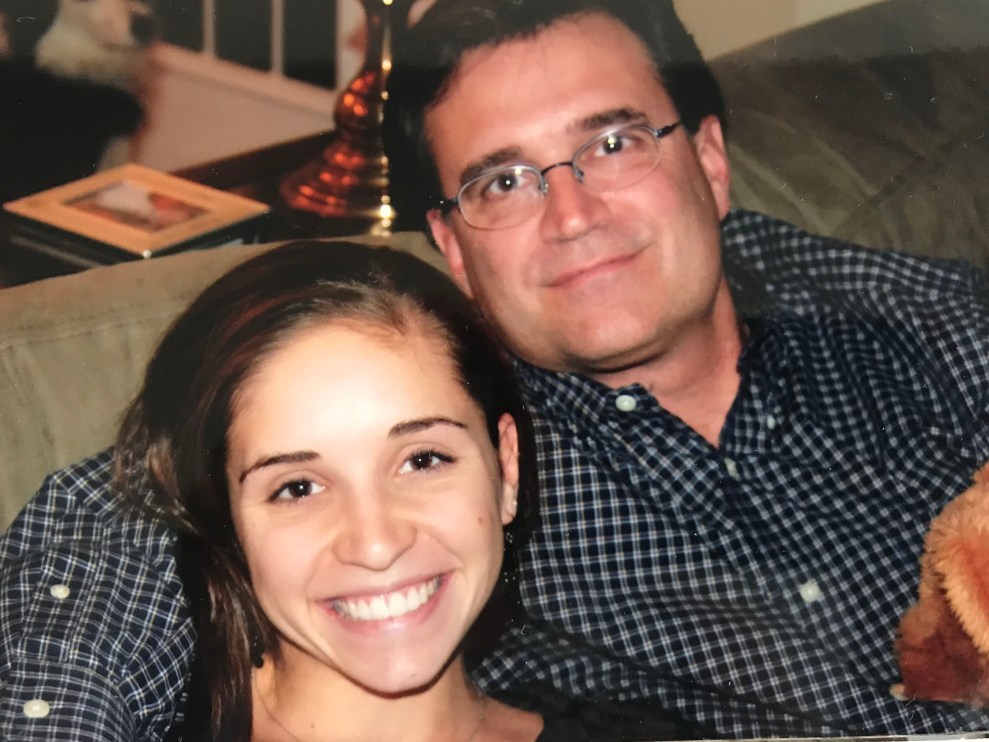
Meredith Legg Stapleton and her father
Courtesy Robin Legg
While she was recovering from her treatment, Meredith got an unusual message. It was from Kenan Colbert Koll, a star swimmer—two years older than Meredith—who was also from Huntersville and attended the same school, Hopewell High School. Her note said that, despite the odds, she too had OM. Kenan first noticed blurry vision in her right eye in early 2009, two years after she had graduated from the University of North Carolina, Chapel Hill. She went to an eye doctor in Charlotte who prescribed glasses, but the problem continued. A few weeks later, she went to Duke University, where a specialist examined her and delivered the devastating news: a dangerously large OM tumor had lodged inside her eye. He offered the same recommendation for standard treatment: removing the eye. Kenan took one breath and commanded, “Take it out!” She had her eye removed at Duke, but, like Meredith, went to Wills Eye Hospital in Philadelphia for follow-up treatment once her cancer began to spread.
Meredith and Kenan became friends and collaborators, seeking new treatments and raising money for OM research. Meredith also coached Kenan on what to expect from her first appointment with Dr. Takami Sato, a medical oncologist at Wills Eye Hospital and one of the world’s top experts in OM treatment. “At Wills, the doctors would give her an immunotherapy cocktail to knock back the cancer,” Kenan’s father, Kenny Colbert, recalls, sitting in his family room near a table dominated by a wedding photo of Kenan, radiantly happy, wearing pearls and a ruched white dress. “They would inject it in her femoral artery and if the tumors glowed it was working.” Kenan brought her laptop into the treatment room each time intending to work, but she’d just laugh and doze off, Kenny says. “The next day she’d get up and just go out and live her life.”
Both young women did go out and live their lives. Kenan was married six months after her first eye surgery. The couple settled in Charleston and fixed up their first house while Kenan worked as an HR specialist at a flooring distributor. Meredith also married, in 2012, and even appeared on the reality TV show Say Yes to the Dress. She also appeared in Dear 16-Year-Old Me, a 2011 documentary on melanoma and the importance of early detection.

Kenan Colbert Koll with her father, Kenny.
Courtesy Sue Colbert
All the while, Meredith and Kenan also endured grim treatments and setbacks. They relied on their own little support group, continuing to swap insights about treatment and new information about the disease. Then, in late 2013, the support group grew: 19-year-old Summer Heath, another Hopewell High graduate, reached out to Meredith and Kenan through a friend on Facebook. Summer described the ordeal of blacking out from migraines in July 2013 and eventually losing sight in her right eye. A retinal specialist in Charlotte confirmed that she too had OM. When Summer and her parents consulted a local radiologist, he said he knew of two other girls from Hopewell High with the same disease. The three bonded immediately.
“Well, it was weird: three girls from the same high school, and OM is an old men’s disease and it doesn’t happen to young girls,” Summer recalls. “We started talking and our families started talking and…we started to investigate.”
By February 2014, Meredith’s cancer had spread. Thin and in pain, she nonetheless painted her nails “Carolina blue” with sparkles and put on a blue shawl to attend a UNC–Duke basketball game with her husband and parents. Two days later she slipped into a coma. Two days after that, she died. She was 26 years old.
Kenan died four months later in May 2014—just one month shy of her 29th birthday.
Summer was devastated. “It’s survivor’s guilt that I feel. My feeling was it should have been me,” she says. “It’s been a really dark place to be, especially after Meredith and Kenan passed away.” But soon, Summer recalls she found a reason “to get through the guilt”: two more young women in the Hopewell community who also had an OM diagnosis.
Meredith, Kenan, and Summer all lived within a few miles of each other in Huntersville, North Carolina, a suburb just north of Charlotte in Mecklenburg County; it’s one of the upscale communities dotting the 500 miles of shoreline surrounding Lake Norman.
Within the relatively young, prosperous population, news of Meredith’s and Kenan’s deaths spread fast in the summer of 2014. It turned out the young women weren’t isolated cases. “By mid-2013 word was traveling on Facebook, and we started to pick up names of other young people [in our area] getting ocular melanoma,” Kenny Colbert says. “By August 2014, we had seven or eight names.”
One of those names was Vicki Kerecman, who was diagnosed in 2011 in her early 30s. When Summer found her after both Meredith and Kenan had died, she says, “Vicki was my sign not to give up, to continue the research.” Then Summer found Courtney Benson, age 29, who got the same diagnosis that year. Neither of the women attended Hopewell High, but both lived within a few miles of the area.
By 2017, physicians would document a total of 18 OM cases among people who lived, worked, or spent time within a 15-mile radius of downtown Huntersville and northern Mecklenburg County. Nine of the first 12 victims identified would be female, and six would be younger than 30. At least five would die from the disease. Today, depending on the vagaries of statistical reporting, patient disclosure, and spotty cancer registries, around two dozen people in the greater Mecklenburg and surrounding counties of Lake Norman in central North Carolina have been diagnosed with OM.
“When Kenan was diagnosed we had never heard of ocular melanoma before,” Colbert says. “But then we heard about Summer Heath getting the disease, and then Courtney and Vicki. The research I pulled off the internet said the typical OM patient would be 50 years or older. It was off the charts for a female to get it.” According to an oncology textbook, “an excess risk of uveal melanoma has been reported in some studies in a variety of occupations” such as welders, farmers, chemical workers, cooks, cleaners, and laundry workers, but there is no explanation for why. Clearly, young female athletes don’t fit the demographic.

Summer Heath presented with a scholarship for Kenan’s Foundation by Kenny and Sue Colbert.
Courtesy Sue Colbert
Meanwhile, a similar mystery was unfolding in Auburn, Alabama, though this ocular melanoma outbreak appeared even more extensive. Juleigh Green, Ashley McCrary, Allyson Allred, and Lori Lee all attended Auburn University and three were sorority sisters in the late 1980s. Over the next 20 years, all implausibly developed OM. In 1999, when she was 27, Juleigh noticed bright flashes of light; she was diagnosed with OM in her left eye. At the time, she knew no one who had the cancer or could talk about it. Then in 2001, Allyson, then 31, also noticed bright flashes, and her doctor discovered a 10 mm OM tumor pressing on a detached retina. Both women’s eyes were surgically removed. Then Ashley, whose husband’s pet name for her was “sweet eyes,” discovered a spot on her iris in 2012. Her right eye was also taken.
Like Meredith, Kenan, and Summer, Ashley was treated at Wills Eye Hospital. When she described the “crazy fact” that she knew two other classmates with the exact same disease, Dr. Marlana Orloff, an ocular oncologist, was shocked. “This isn’t normal,” Orloff told Ashley, noting that the Hopewell High School classmates had also come to Philadelphia for treatment. “The fact that in two separate areas there were younger women who knew other young females with [OM] has really piqued our interest.”
Summer’s mother, Janie Slusarick, had a similar experience when she accompanied her daughter on her first visit to Wills. When she told their doctor that three girls from the same high school had the same cancer, he froze. “It was like a deer in the headlights,” Slusarick recalls. The OM specialist noted that he was treating others with OM from Huntersville, along with a group of three women from Auburn, Alabama.
Dr. Miguel A. Materin, director of ophthalmic oncology and a specialist in radiation treatment of eye cancers at Duke Eye Center, also found the number and nature of cases concerning. “Something is going on, but nobody knows the reasons,” he says. “Three girls from the same Huntersville High School? That’s not a coincidence. The same thing in Auburn, which may be even more interesting because of all these people who have some kind of relationship with the university there.”
So why are all these young women contracting ocular melanoma? The question consumes victims and the OM community. Parents, desperate to discover anything in the environment that could explain what seems inexplicable, struggle to solve a medical mystery in which a tragic diagnosis is followed by questions, accusations, theories, the debunking of those theories, and, too frequently, death. Is it possible to discern a clue in the complicated mix of environmental hazards and genetics that has made these young women particularly vulnerable to disease?
OM is an illness that does not lend itself to clear causalities, like connecting cases of lung cancer to tobacco use. The rarity of the eye cancer has precluded deep study—and funding for research. Epidemiologists say it’s nearly impossible to “nail” a cancer like OM to a single risk factor. This is needle-in-the-haystack stuff: human genetics, immune systems, hormones, and environmental factors have complex interactions. One person exposed to chemical contaminants or high levels of radiation may never develop disease; others will. But that hasn’t stopped efforts to try at least to narrow down areas of inquiry.
One key way to marshal support for research and treatment is to get what’s known as a “cancer cluster” designation from the Centers for Disease Control and Prevention. The CDC designates a cancer cluster as “a greater-than-expected number of cancer cases that occurs within a group of people in a geographic area over a period of time.” With the designation, more public money and research power is made available to find out what’s going on; without it, opportunities both to understand the causes and the treatments for the disease become more difficult. Nonetheless, for complex reasons that are both legal and scientific, it’s almost impossible to pass the threshold of an official cancer cluster designation.
The few success stories that garner public attention read like industry-busting detective stories initiated by rookies. The classic example is Erin Brockovich’s now-famous 1990s investigations showing that hexavalent chromium in the town of Hinkley, California, was triggering various cancers. Her work resulted in a class action lawsuit and settlement of $333 million against Pacific Gas & Electric. Public health officials today cite other outstanding cases of cancer cluster discovery, but the singular, dramatic successes in which an investigation actually uncovers common triggers have centered almost exclusively on infectious disease outbreaks, like Legionnaires’ disease or the discovery of how mercury poisoning was caused by contaminated fish.
Communities across the country raise around 1,000 or more “cancer cluster alarms” each year, according to the CDC. For the designation of an official cluster, epidemiologists compare observed numbers of cases of specific cancers against case records of the same disease in a similar setting with a similar demographic group. At least that’s the goal. But comparisons with similar groups may be over a much larger geographic area, like an entire state. The CDC’s website acknowledges “it is possible to ‘create’ or ‘obscure’ a cancer cluster by selection of a specific [geographic] area.” Time comparisons may also be a crucial variable. The five ocular melanoma cases among young women with connections to Hopewell High School cropped up between 2009 through 2013, whereas North Carolina state epidemiologists compared those numbers to expected cases in the area over 20 years.
Chris Nidel, a health and chemical exposures attorney in Washington, DC, calls this practice “dilution” because statistical models can be used to skew results by comparing cancer or infectious disease outbreaks in a single town or zip code against countywide or several county populations over much longer periods. “Diluting your population means you’re unable to see change at the level you’re wanting to see plainly in a town where people get sick,” he says, especially because “‘cluster’ isn’t the answer you’re looking for. The real issue is: Is there something causing disease in your community?”
Then there are the challenges of investigations themselves. Many cluster investigations are launched without clear objectives—usually in response to general community distress, writes Dr. Michael Goodman, an Emory University epidemiologist, in the journal Critical Reviews in Toxicology. The undesirable result is that “cluster investigations of cancers that appear to arise in a given geographic area or in a given community have rarely, if ever, resulted in important discoveries.”
It’s exceedingly difficult to get local authorities to test environmental factors, and, as a result, public health officials haven’t had much success in linking suspected cancer outbreaks with environmental causes. First, soil and water testing isn’t required in many states, including North Carolina, unless the sites specifically require permits for pollutant discharge under state and federal law. “The investigations are extraordinarily hard to do,” said Catawba Riverkeeper Brandon Jones, a hydrologist. He lists a number of variables involving environmental factors as well as individual medical histories. “These tests can very expensive,” he noted, “and you really do have to know what you’re looking for.”
The Clean Water Act requires the North Carolina Department of Environmental Quality to employ an Ambient Monitoring System whereby the state picks new sites every two years to look for water pollution, according to Jones. But there is no similar mandate for soil. Plus, there aren’t uniform regulations in either states or nationwide for testing for pollutants when townships build schools, neighborhoods, or commercial strips.
Making matters worse is a completely broken case tracking system. Public health officials rely on state cancer registries that are often incomplete and outdated. These registries do not track potential exposure to toxic sources, like polluted groundwater or dumping grounds for industrial waste. State cancer registries also typically use medical shorthand, documenting only the name and current address of the patient, as well as basic demographic information such as age, race, and gender. The tumor diagnosis is marked by code and staging (how far advanced the tumor is) along with initial treatment notes and where the patient lived when first diagnosed. Migration patterns of patients are almost never recorded. Registries don’t include data on toxic exposure in a patient’s formative years—several bad sunburns, say, or DDT sprays in the area. These flaws are evident with the Huntersville cases: Kenan and Meredith were counted only in a South Carolina registry, since that was where they were first diagnosed, even though they spent their high school years in Huntersville. Summer wasn’t included in the North Carolina cancer registry when investigations took place in 2015 because her official data hadn’t as yet “caught up” to registry databases.
National tracking is even worse for OM because of its comparative rarity. Other than an American Academy of Ophthalmology national registry, called the IRIS database, which records many kinds of ocular disease and their incidence rates, no national database has addressed ocular melanoma alone, although one has recently been created.
Even traditional methodology epidemiologists have relied on for their studies may be adding to the problem. In 2012, for example, Michael Goodman, the Emory University epidemiologist, reviewed 428 cancer cluster investigations evaluating 567 suspected community outbreaks. Of those, only 72 clusters, or 13 percent, demonstrated an increased cancer incidence beyond what was expected for the community studied. Only three of the cluster investigations were actually linked, “with variable degrees of certainty,” to a hypothesized exposure to a specific environmental trigger, while only one investigation out of the 428 revealed a clear cause. With all this data, the limited results suggest that there may be a fundamental problem in how causality is framed, especially when it comes to identifying possible environmental triggers for health outcomes.
The challenges in cancer cluster designations have proved so daunting that Goodman and Judy S. LaKind, a professor of epidemiology at the University of Maryland Medical School, assembled a workshop to review past cases and offer new approaches. In a 2014 report, the researchers cited statistical problems such as small sample sizes, uncertain definitions of cluster boundaries and populations, and a failure to record the in-and-out migration from a suspicious area by patients. Too many cluster studies, they found, also use imprecise descriptions of both disease states and potential environmental factors. For example, public health officials might use the term “brain cancer” to describe a specific diagnosis such as glioblastoma. The term “ground water contamination” might be reported instead of the specific levels of trichloroethylene, chloroform, or dioxins. Some suspected clusters are just too small to calculate, with exposures to toxins by the community poorly defined or undefined. Then there’s the pace of the disease, known as latency. Cancers develop over a long period of time—often a decade or more—making associations with suspected toxins much more difficult to prove.
Because of the way North Carolina public health officials counted victims in their studies, the Huntersville cases didn’t reach an official “cluster” incidence level, according to a 2015 state public health report. The families were left grieving and infuriated. Emotions ran even higher when an official cancer cluster was determined in Mooresville, just a few miles north of Huntersville on Lake Norman, when thyroid tumors appeared in as many as 260 local victims, most of them young women and teens as young as 13. The aggregate burden of investigating both outbreaks has produced community anger and cries for help from state legislators. To many residents, Lake Norman has become a “cancer alley” with too many industrial contaminants and too few public health resources to investigate and find answers.
“The numbers just don’t make sense,” says Rob Kidwell, the father of a school-aged daughter in Huntersville. “These are rare cancers that shouldn’t be popping up and no one seems concerned.”

Kenan Colbert Koll
Courtesy Sue Colbert

Meredith Legg Stapleton
Courtesy Robin Legg
When I meet with Kenan Colbert Koll’s parents, Sue and Kenny Colbert, at their Georgian-style retreat tucked away in a verdant Huntersville neighborhood, we’re joined by Scot and Janie Slusarick and their daughter, Summer Heath. It’s June 2018, and Summer, 24 years old and teaching second grade, is about to celebrate five years of surviving OM. Summer has a blog, Cupcake v Cancer, where she shares what has been happening to her. Entries about her care, like one from last year—“I think the treatment is working though. The tumors on my head have been shrinking. That is an amazing reassuring sign that we are headed in the right direction!!”—are mixed with photographs of friends and trips to Disney World. When Summer speaks, she expresses both sadness and a fierce will to live.
By that June, Summer had already made 23 trips to Philadelphia for plaque therapy, biopsies, painful injections, and lasers to destroy her tumor. Months of radiation were followed by a laser to kill any cells left, then a series of injections to stop macular swelling, followed again by laser treatment in 2016 to halt hemorrhaging in her eye, which had lost all vision. “Our cases—Meredith’s, Kenan’s, and mine—are so similar, there’s a bond there,” she says. It’s been hard on her family; her medical insurance had paid only a fraction of her bills. But it helped when her friends gave her hotel points so she and her family could stay in Philadelphia as an outpatient for the first 10-day course of treatment.
The Colberts and Slusaricks listen as she speaks before describing their arduous four-year journey of false hopes and dead ends as they tried to get local and state officials to take environmental testing seriously. In 2014, Scot Slusarick thought that one obvious common denominator was location: Three of the girls with OM attended Hopewell High and two young women in their 30s lived within a mile nearby. He lobbied public health and school officials for a physical sampling of the Hopewell High water, soil, radiation sources, and air, but officials declined his requests.
At the same time, Kenny Colbert was prodding the Mecklenburg County Health Department to initiate a cancer cluster study. In March 2014, just months before Kenan died, Colbert connected with the county health director, Dr. Marcus Plescia, who phoned OM victims, families, and school officials, asking questions about potential toxic exposures and lifestyles, like work as lifeguards, sunburns, a history of smoking, or use of artificial tanning beds. Nothing suspicious was found, according to the county health department office.
While the county inquiry stalled, Colbert enlisted Huntersville Township Commissioner Danny Phillips and former Commissioner Rob Kidwell, as well as his wife in his search for answers. The Kidwells, like Slusarick, pressed hard for physical tests of the air, water, building materials, and soil at Hopewell High. They also tried to survey the townships nearby to establish baseline pollution data, but there was no consensus on how to proceed, Kidwell recalls. “The state said it was a county issue; the county said it was a state issue,” and nothing got done, Colbert says. Eventually state epidemiologists told Colbert that “five cases in your area over the last 20 years” was normal. “We have five people within a one-mile area right now,” he countered, referencing Meredith and Kenan, who had already died, plus Summer, Vicki, and Courtney. “The state said, ‘We don’t know about these five people. There’s no central registry.’”
But Colbert worked to bring attention to the cause in other ways. He called local TV reporter Jim Bradley, who started looking at whether state and county health officials acknowledged a potential problem. His first report aired in November 2014, and soon other Lake Norman community members claimed an OM diagnosis. “Word started traveling and soon we had about 25 names within six to seven miles,” Colbert reports. Following that publicity, in late September 2015, the Colberts, Slusaricks, and other members of the Huntersville community participated in a “Lookin’ for a Cure” 5K walk/run to benefit Dr. Takami Sato, director of the uveal melanoma treatment program at Wills Eye Hospital. Dr. Sato showed up at the Huntersville run, along with his son and Dr. Marlana Orloff, who had treated both the Huntersville and Auburn women. About 1,000 people participated in the event, which raised more than $55,000.
Beyond fundraising, the run proved crucial for another reason: Dr. Randall W. Williams, the deputy secretary of health services at North Carolina’s Health and Human Services, was there. Williams had spoken with Colbert and decided he needed a clinical liaison to speak to OM parents in Lake Norman. The plan was to organize a consortium of Duke, Thomas Jefferson, and UNC, Chapel Hill, experts to figure out next steps for an exploratory study.
Williams selected Dr. Mike Brennan, a retired eye surgeon and colleague of his who’d done overseas medical work in Iraq, Libya, and Afghanistan. “Randall called me about OM in Huntersville,” says Brennan, who is also the former president of the American Academy of Ophthalmology, “and he said, ‘You know how to do ocular politics, can you help me?’” At the time, Brennan admitted he didn’t know much about the Huntersville cases, but he agreed to sign on and organize a local registry of the Lake Norman OM patients. He told Williams the consortium should coordinate genetic testing of victims and, possibly, an environmental study of Huntersville.
As Brennan started contacting patients in late 2015, he found that patients were scattered in and around the counties surrounding Lake Norman. He almost immediately found at least three more young people in Huntersville and nearby Concord and Lincolnton, all near Lake Norman, who had reported the disease in the same timeframe, along with two older patients. But the process hit some snags: Some patients had privacy concerns and didn’t want to be included in the registry. Counting cases was also difficult because “there were people who were diagnosed before 2000, or their geography was wrong, or they were transients,” Brennan says. But, he adds, “the [patient] population grew as social media and the press publicized this.” In the end, Brennan documented at least two dozen OM patients for his Lake Norman registry, although a few were excluded because their time and place of diagnosis didn’t fit standard epidemiological requirements. UNC, Chapel Hill, found two more patients, one from Huntersville and another from Rock Hill, South Carolina, who had worked in Huntersville for five years. One of the last patients to be registered was Jessica Boesmiller, a mother in her late 30s whose OM was detected in late 2017, just weeks before delivering twins.
Meanwhile, officials at the North Carolina Department of Public Health’s Occupational and Environmental Epidemiology Branch (OEEB) published a report in June 2015 on the OM cases. It concluded that other Lake Norman cases were random, albeit tragic, events. According to Kelly Haight Connor, a spokesperson for the state health department, “An analysis of NC Central Cancer Registry (CCR) data in 2015 did not find a higher-than-expected number of ocular melanoma cases in Mecklenburg County, Huntersville or Huntersville/Cornelius from 2000–2013.” (Physicians and epidemiologists from the state health department declined to be interviewed.) When the findings began to circulate, Huntersville parents were outraged.
Janie Slusarick called the OEEB report naive and embarrassing. “There are two to three times the numbers of people affected here and the state report doesn’t count them,” she says. “From my perspective,” Brennan adds, “I could tell that for good reasons, the community and parents had reason to expect more to be done.”
The Slusaricks continued to press for environmental testing of the school. In 2016, facing pressure from the Huntersville community, the school system finally agreed to a first investigation of construction records and a visual inspection of Hopewell High School grounds by Hart & Hickman, a Charlotte-based environmental consulting firm. Nothing unusual was detected, and H&H didn’t recommend any soil or water tests for contamination, arguing its own chemical records search showed no single link to OM.
Scot Slusarick then pressed Charlotte-Mecklenburg facilities management to evaluate Hopewell High’s tons of imported fill dirt and building materials, but the department claimed that supervisors had already reviewed construction records when the high school was built in 2001. “What about the paint? The ceilings? The lighting?” he asked. “Their entire investigation was a phone call.” Janie pointed out that the area historically had copper mines and water tributaries running from them. She also noted that a mile and a half from school was a Piedmont liquefied natural gas storage facility, which could possibly be emitting harmful electrical pollution—sometimes known as “dirty electricity.” That too should have been evaluated, she says.
While environmental testing was stalled, Brennan believed that genetic testing might yield important clues. He coordinated a test of local victims to determine if anyone had the BAP1 gene mutation, a protein abnormality frequently associated with eye, skin, and kidney cancers. But all tests were negative. Even after experts from Columbia University, the New York Genome Center, and the University of Miami’s Bascom Palmer Eye Institute participated in tumor tissue testing of six North Carolina patients, there was no “smoking gun.”
Another option was geospatial testing, which links patient activity and remembered traffic patterns with repeated exposure to toxic environmental sources such as radiation or air and water pollution. In 2017, Huntersville Township funded a study by an environmental consulting firm, Geodesy Inc., which specializes in geospatial testing. The remembered whereabouts and daily traffic patterns from 2000 to 2017 of 11 female and four male OM patients living within the Huntersville ZIP code was mapped and then correlated with township records that revealed various “hot spots” in Northern Mecklenburg County: an asbestos dumping site at Davidson Depot; a dry cleaning solvent clean-up site in Huntersville; several active hazardous waste storage facilities in the north; contaminated industrial sites in both Cornelius and Huntersville. It also showed the presence of polychlorinated biphenyls in Lake Norman, which provides public drinking water to Huntersville, and a concentration of high-tension power lines, cell towers, and power-generating stations in the vicinity.
The report stated, “Without important clues, additional measures of air, soil, or water is not warranted.” Still, Geodesy report director John Cassels called for further analysis of multiple sources, including Lake Norman public water. Both coal ash and nuclear radioactivity are common sources of pollution across all modern towns in the US, and coal ash often appears in water supplies—including Lake Norman. Avner Vengosh, a professor of earth and ocean sciences at Duke University’s Nicholas School of the Environment, has in fact documented coal-ash effluent in all the major lakes and streams connected to coal-fired power plants throughout North Carolina, including Lake Norman. But he notes that because of the lake’s gargantuan size, dilution is large and the impact is small. Municipal water quality tests of the lake have not shown hazardous levels of any coal-ash chemicals or radioactivity.
Despite missing a clear culprit, Geodesy Inc’s director, John Cassells, admits he was a “little bit alarmed” at some of the things their investigation found. Duke Energy, for example, had an unplanned release in 2008 of the hydrogen isotope tritium from its McGuire Nuclear Station near Huntersville, which amounted to 140,000 gallons of tritium-tainted water flowing into Lake Norman.
While tritium is a radioactive compound found in nuclear reactors, Duke has regulatory permission to release tritium and other effluents into the Catawba River, which flows into Lake Norman. The unplanned leak, a Duke spokesperson wrote in an email, “did not impact public or employee health and safety.” Duke Energy’s director of government affairs, energy and the environment, Mark McIntire, says that tritium isn’t dangerous in low doses and that Duke strictly follows toxicity-based standards for water quality established by EPA and North Carolina’s Department of Environmental Quality. Bill Norton, a spokesperson from Duke Energy tells me, “We have environmental discharge limits and have to report all that data to the nuclear regulatory commissions…The Lake Norman water quality remains very good.” In a later conversation he adds, “Decades of environmental data at drinking water intakes show no impacts from our operations.”
Tritium concentrations in Lake Norman remain below federal limits. Duke notes the calculated radiological impact of that leak on an individual was equivalent to .00005 millirem—or just 1/10,000th of a dental X-ray. But Cassels is still concerned. “There are several drinking water intakes downstream [from the McGuire Station] and no way to clear these compounds,” he says. “Even low concentrations of tritium may be more important in cancer than we originally thought.”
There are some reasons for hope: The efforts to achieve a national and international registry of OM cases are rapidly coming to fruition. The Melanoma Research Foundation has created a new kind of patient-centric registry that will help disease detectives track the natural history of eye melanomas, including environmental risk patterns, treatments, and recovery. Dr. Sara Selig, a physician who directs “Cure OM,” the Melanoma Research Foundation initiative, explains, “What’s hindered the research into some of these unique populations in the past is that you know someone who may have lived in one area and been diagnosed somewhere else, and there’s not a single repository catching this information. What’s the unique factor? The person.” She says that instead of the standard clinical data provided by physicians, a new repository will allow patients to enter remembered environmental exposure data, migration patterns, family histories, and responses to treatment across the lifecycle of the disease.
Academic researchers hope to find clues to OM causes in these records and in victims’ genomes. At Columbia University’s Irving Medical Center, Dr. Richard Carvajal, a director of experimental therapeutics, is conducting a whole genome sequencing study of both the North Carolina and Alabama OM patients, examining tumor tissue for patterns of genetic damage. “There are about 30 DNA ‘damage signatures’ that have been characterized, and are pretty well accepted,” says Dr. William Harbour, a consultant on the project and a genetics researcher at University of Miami’s Bascom Palmer Eye Institute. Harbour is optimistic; a genetic pattern may narrow down environmental causes and point to one or more smoking guns. “There’s a lot of reasons to think this eye cancer isn’t coincidental,” he says. “Some people are concerned with legal implications, and maybe they don’t want to find [the answers]. But from a government standpoint, your best bet is to show you’ve made every reasonable effort to find the cause.”
Even though the Huntersville community search for an OM cause seemed inconclusive, there is movement on attempts to get to the bottom of the Alabama cases. In August 2018, Auburn University also engaged Geodesy Inc. for a geospatial investigation. According to Cassels, the work has been delayed because of the coronavirus pandemic, but it could still turn up some promising data. The geospatial analysis will dig into genetic, lifestyle, or environmental causes of the disease in the Auburn community. It will focus on the 25 surviving patients out of the 31 who were confirmed to have the disease and affiliated with the school from 1980 to 2019.
Ashley McCrary, the Auburn grad who was diagnosed with OM in 2012, says, “The geospatial engineer is going to come in and ask a thousand questions to everybody [regarding remembered whereabouts, exposures, and life style habits] and pray that people will send the information back.” Dr. John Mason, a retinal specialist based in Birmingham who treats many of the Auburn patients, is optimistic that this study, which includes more patients and looks at a longer time frame than past research, will also yield important clues.
Still, the Colberts and Slusaricks remain haunted by the painful question: How can public health officials be fully aware of these cancer outbreaks and not know what to do? Back when Kenan was still alive, Kenny Colbert wanted to get the community riled up, to change the attitude of public health officials who seemed not to want to look more carefully at a problem that could make other young people sick. “We needed to get people mad and scared about this,” he says. “We decided we should get some people embarrassed about this, about doing nothing or passing the buck.”
The battle also continues for patients like Summer Heath and Jessica Boesmiller, the young woman whose cancer was discovered just before she delivered twins. Summer shuttles back and forth to Wills Eye, as well as to Duke, for treatments, now for brain and spinal tumors. But she still keeps her blog. She still teaches second grade at Langtree Charter Academy Elementary School. And she recently celebrated seven years of survival since her diagnosis, as well as her 26th birthday.
Jessica also regularly travels to Wills, in between the demands of raising her four kids, to treat the cancer that has metastasized to her spine and liver. She reflects on her experience from two perspectives: first, as a fierce advocate for changing the usual approaches to understanding the cause of this devastating disease. “Everyone investigating ocular melanoma is too worried about liability to say what the cause could be without [assembling] clear evidence,” she says. “But I want full disclosure—full access and open testing of the environment. If the old ways of finding out what’s wrong don’t work, find a new way. This cluster is just too coincidental to be a coincidence.”
At the same time, Jessica has the perspective of a young woman, a daughter, a wife, and a mother whose life has been unalterably changed and defined by her battle with OM. “People ask how I feel and it’s difficult to express sometimes. My family sees the pain and lack of energy and physical strength. They see the tiredness and nausea. They miss the old me,” Jessica says, “and I really do.”