When Catherine was in her late 20s, she and her husband decided to start a family. She had always assumed it would be easy—her friends seemed to get pregnant without even trying. But after three years, she still didn’t have a baby. A fertility specialist prescribed medications. They didn’t work, so the doctor tried inserting Catherine’s husband’s sperm directly into her uterus, a procedure called intrauterine insemination. Still no luck. “I felt like a failure,” she later wrote on her blog. “Even with medical assistance I couldn’t complete the one task that my body was created for. I could have filled buckets with the amount of tears I cried.”
She tried a few more rounds of artificial insemination, and when that didn’t work her doctor suggested in vitro fertilization (IVF). The thought of more procedures and drugs exhausted Catherine, and her fertility medications made her prone to wild mood swings and fatigue. So when a friend recommended a different kind of fertility expert, Catherine was all ears. Her friend had been seeing a doctor who practiced a technique called NaPro, short for “natural procreative technology.” She assured Catherine that the NaPro doctor could determine the underlying cause of her infertility—which Catherine’s current doctor had never been able to do.
Catherine, who asked to have her name changed to protect her privacy, began to research NaPro. She was impressed: Its practitioners claimed it was more effective than IVF and cost only a few hundred dollars—practically nothing compared with the tens of thousands for a few rounds of IVF. Catherine made an appointment with the NaPro doctor, who instructed her over the phone to chart the changes in her cervical mucus over the course of her menstrual cycle. At her first appointment, after looking at those charts, the doctor told her he was “90 percent sure” she’d been suffering from endometriosis, a painful condition where cells from the uterine lining grow outside the uterus.
The American Congress of Obstetricians and Gynecologists (ACOG), the professional group for doctors who specialize in women’s reproductive health, does not advocate aggressively operating on endometriosis as a way of improving fertility. The condition may return, and surgery can cause scarring that can prevent or complicate pregnancy. Catherine’s NaPro doctor recommended exploratory laparoscopic surgery, after which, he said, she’d have a good chance of having a baby. He offered to pray for her in church; Catherine, a practicing Christian, was touched.
Several months later, she traveled to a NaPro surgeon who treated her endometriosis. Catherine finally got pregnant nearly a year later, but her joy was short-lived: She miscarried at eight weeks. Her NaPro doctor prescribed more vitamins and medications and urged her to continue charting.
Five years after her first NaPro appointment, Catherine still didn’t have the baby of her dreams. “I don’t make resolutions,” she posted on Facebook one New Year’s Eve. “I work every hour of every day to become a mommy.”
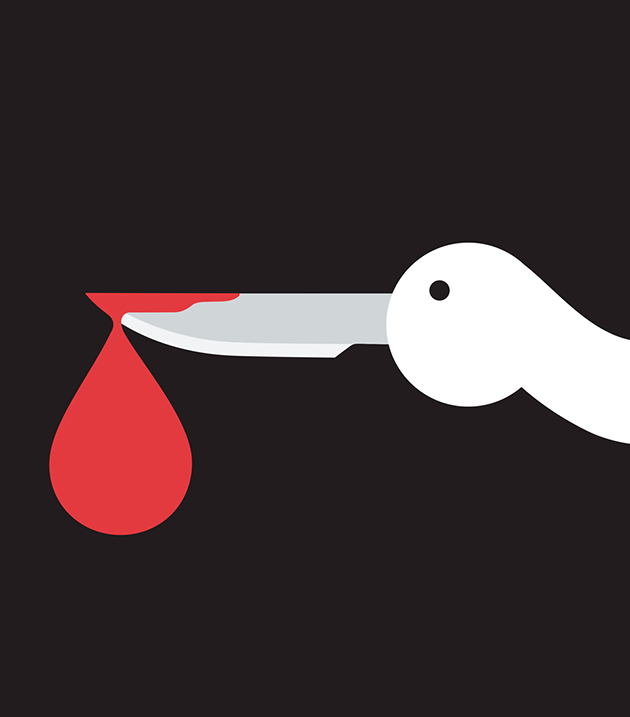
The Scary Truth About Childbirth
Catherine’s doctor was part of a growing movement that offers women a medical and moral alternative to IVF. Tucked away in a brick-lined office building in Omaha, Nebraska, is the Pope Paul VI Institute for the Study of Human Reproduction, the home of NaProTechnology. Its founder, Dr. Thomas Hilgers, is an obstetrician and a devout Catholic; he developed the practice in the mid-’80s, around the same time the Vatican denounced artificial insemination and test-tube babies. Hilgers, now 74, says his method—which typically involves some combination of mucus charting, blood tests, transvaginal ultrasounds to monitor ovulation, fertility medications, and one or more exploratory surgeries—has helped thousands of infertile women get pregnant. He claims that NaPro’s success rates are more than twice those of IVF.
With its growing network of 300 FertilityCare Centers, Hilgers’ institute positions itself as the go-to solution for couples who are fed up with mainstream fertility techniques or believe they are immoral. In the last decade, Hilgers’ practice has spread to at least 10 countries on five continents. In 2015, the Polish national health care system quit funding IVF in favor of NaPro. As the website of a NaPro center in California declares, “You don’t need IVF.”
It’s not hard to see why NaPro appeals: Practitioners present it as a medical breakthrough. “Thirty years of scientific research in the study of the normal and abnormal states of the menstrual and fertility cycles have unraveled their mysteries,” the NaPro website states. The Pope Paul VI Institute boasts a state-of-the-art lab and a network of skilled surgeons. It offers a fellowship program for obstetricians. On his websites and in his writing, Hilgers cites dozens of studies and charts that suggest his decades of work have yielded impressive results. He claims nearly 100 percent of his patients with certain infertility-related conditions eventually get pregnant.
There’s just one problem. Scant medical evidence supports Hilgers’ lofty statements about pregnancy success rates, according to leading reproductive endocrinologists. Most of the research that Hilgers cites is self-reported; the only peer-reviewed studies are by a NaPro practitioner and medical school professor in Utah. I shared his studies with Dr. David Adamson, a clinical professor at Stanford University and the former president of the American Society for Reproductive Medicine. Adamson pointed out that the studies were small and did not control for variables that might have influenced the results. Those results, Adamson wrote in an email, are “not replicated in any other studies and are not believable when compared with multiple good studies.” What’s more, he said, he hasn’t seen sufficient evidence that NaPro works any better than simply trying to conceive a child by having sex regularly.
Hilgers “is not practicing evidence-based, 21st-century Western medicine,” says Dr. Richard Paulson, chief of the reproductive endocrinology and infertility division at the University of Southern California Keck School of Medicine. Paulson points out that while NaPro may be cheaper than IVF, it’s not without cost. Many NaPro patients spend several years undergoing treatment. “While you are waiting for this to kick in, you’ve lost years off the biological clock, which is a high price to pay,” Paulson says. The reproductive endocrinologists I spoke with also expressed deep skepticism about NaPro’s reliance on exploratory surgeries. An ACOG spokeswoman wrote in an email that her group “has numerous clinical guidelines based on scientific research and evidence on issues of fertility and gynecologic health, but NaProTechnology is not among them.”
But Hilgers, who did not respond to requests for an interview, is not trying to impress mainstream fertility experts. In his 2010 book, The NaProTechnology Revolution, he dismisses ACOG as an industry shill whose members are in the pocket of “the pharmaceutical industry that supports contraception, sterilization, abortifacient medications, and in vitro fertilization.” That tirade is part of his larger case against artificial reproduction. He describes artificial insemination as “a technique where the physician usurps the role of the husband or father,” denigrating “both marriage and parenthood.” What’s more, “it has been used to impregnate single women and lesbians.” IVF is even worse, because it is “creating life through destroying life” by producing embryos that eventually get discarded. Such technologies, writes Hilgers, are the “giant” to NaPro’s “David.” He thunders against contraception, arguing that it has caused an epidemic of sexually transmitted diseases, depression, and suicide. NaPro is also entwined with the anti-abortion movement. Many “crisis pregnancy centers” that discourage women from having abortions offer NaPro.
Yet NaPro isn’t limited to Catholic hospitals and anti-abortion medical clinics. Doctors affiliated with public universities, including the University of Utah and the University of California-San Francisco, use Hilgers’ technique. In Wisconsin, a practice run by the renowned Mayo Clinic provides NaPro, as did a US Navy hospital in Jacksonville, Florida. Many graduates of the Pope Paul VI Institute’s training program work in mainstream facilities, and NaPro doctors are board certified.
Take Christopher Stroud, a NaPro doctor with a thriving practice in Fort Wayne, Indiana. Stroud had been an OB-GYN for more than a decade when he converted to Catholicism and decided to stop referring patients for IVF. “I struggled a long time and finally came to the conclusion that I could not keep doing it,” he told me. “But I didn’t feel like I could do that without a replacement.” He learned about NaProTechnology and enrolled in Hilgers’ training course. Since he became certified to practice NaPro, he says he’s treated hundreds of patients, some of whom drive five hours to see him. Stroud says that after they’re evaluated for three to six menstrual cycles, 85 percent of his patients get pregnant within three to six months—though he wouldn’t share records of his success rates. He incorporates his faith into his practice, urging unmarried couples to tie the knot and praying with patients before they undergo procedures. Prayer is “a big part of my approach to my surgeries,” he says.
Stroud typically doesn’t ask patients about their religious beliefs, but he has a feeling that most seek him out either because they’re ethically opposed to IVF or because they can’t afford it. That last point is key: Neither Medicaid nor most insurance plans cover infertility treatments. Yet almost all of NaPro doctors’ infertility-related procedures and medications are covered by patients’ insurance plans or Medicaid. That’s because they submit claims for treating the underlying conditions they think are preventing their clients from getting pregnant. “So a woman might say, ‘I want to get pregnant,’ and I would say, ‘Do you have painful periods?'” Stroud explains. “In that case, they probably have endometriosis. That’s a disease.”
NaPro practitioners also claim they can cure a host of other reproductive problems. Natural Womanhood, a Hilgers-affiliated clinic in San Antonio, Texas, informs prospective patients that its method is “95.2 percent effective” for treating PMS; a NaPro center in Connecticut boasts that “improvement is often observed within hours” after its hormone-based treatment for postpartum depression. The claims about NaPro’s ability to prevent miscarriage are the most outlandish. The current medical consensus is that up to a quarter of all pregnancies end in miscarriage, and that most are caused by chromosomal abnormalities in the embryo and are unpreventable. Hilgers disagrees. “We are slowly coming to recognize that no miscarriage can be considered normal,” he writes. “All miscarriages are the result of an abnormal reproductive event.”
Despite scientific evidence to the contrary, Hilgers believes that doctors can prevent miscarriages, PMS, preterm labor, and postpartum depression simply by administering the sex hormone progesterone. Adamson points out that even though progesterone is well studied, there is no scientific consensus on whether it helps with the array of conditions that Hilgers claims it does. “The evidence doesn’t support that,” Adamson says. “It’s not appropriate to recommend it for everybody.”
But much of NaPro’s appeal comes back to Hilgers’ assertions that it is more effective than IVF. However, the data he uses to make these comparisons is suspect. On the NaPro website, a chart comparing NaPro and IVF pregnancy success rates draws mostly on data from 1986, when IVF was still experimental. Hilgers laments IVF’s high rate of twins and triplets, who are likelier to be born prematurely and less healthy than single babies. Yet he fails to mention that the rate of multiples born from IVF has plummeted; most reproductive endocrinologists now prefer to implant one embryo at a time. “To say the [IVF] field has come very far since the ’80s is a major understatement,” says Paulson. “It’s just been light-years in terms of science.”
It is true that IVF is by no means a miracle cure for infertility. Only about 30 percent of women who undergo one round of treatment deliver healthy babies. For women in their late 30s and 40s, the success rate is much lower. That is exactly why NaProTechnology’s claims of success, combined with its spiritual gloss, are so alluring. Infertility forums and blogs are full of women who are sure their patience with NaPro will soon be rewarded. “I know one day I will look back on this trial and be like, ‘that’s why you allowed this trial, that’s so good it didn’t happen then!'” writes one blogger who has been a NaPro patient for four years. “Or maybe be so much better than I imagined and worth the wait. Maybe it will be twins!”
Even after years of waiting, Catherine still credited her NaPro doctor for curing her endometriosis. “You can’t say NaPro didn’t work for me,” she said. “It’s because of NaPro that I have an active life.” She had started looking into adoption, but just before this article went to press, Catherine shared some wonderful news: She was a few weeks pregnant. I asked her how she was feeling. “I am completely terrified because of what happened before,” she admitted. Still, she remained optimistic. “I feel different this time. I am very hopeful.”