Nathan Howard/Getty
The Delta variant is here. And as it continues its spread across the globe, the media has been in a frenzy. Last week, for instance, reports circulated about vaccinated individuals in Israel who became infected with the new variant. We saw headlines about the rise in COVID cases driven by Delta in the UK, and news of six vaccinated people dying of COVID in the Seychelles. Meanwhile, Los Angeles and the World Health Organization are advising the vaccinated to return to masking indoors.
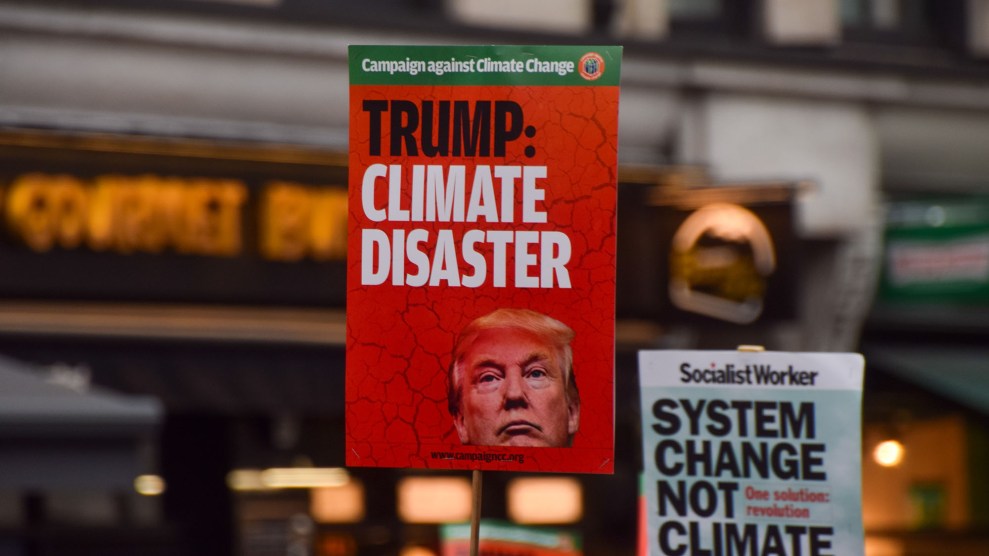
The news, frankly, is scary—and confusing. Making matters worse, anti-vaccine groups have begun to weaponize the confusion for their own gain. Some of their claims are just flat-out wrong: One bit of disinformation making the rounds is that people who are vaccinated are at a higher risk of dying from COVID caused by the Delta variant—an unsubstantiated assertion that has been debunked.
Other anti-vaccine activists are exploiting statistics without important context. Robert F. Kennedy Jr.’s anti-vaccine group, Children’s Health Defense, issued a write-up about recent CDC data showing that about 4,115 fully vaccinated American patients who tested positive for COVID had been hospitalized or died of as of June 21. What the piece didn’t say is that more than 150 million people in the United States had been fully vaccinated at the time—making these “breakthrough infections” very, very rare. It also failed to mention that experts say breakthrough infections are expected, and that data indicates that most breakthrough cases are asymptomatic or mild.
To set the record straight—and hopefully, relieve some of your stress—I picked the brains of three experts: Dr. Shira Shafir, a professor and infectious disease epidemiologist UCLA’s Fielding School of Public Health, Dr. Monica Gandhi, a professor of medicine and an infectious disease physician at the University of California, San Francisco, and Dr. Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine and co-director of the Center for Vaccine Development at Texas Children’s Hospital.
While the Delta variant is worth taking seriously—it does spread more easily than the “ancestral strain” of SARS-CoV-2—they told me, there isn’t enough evidence that it is deadlier than other strains. Crucially, they emphasized that the vaccines are proving to be powerful tools against Delta and other variants of this virus. And those stories about breakthrough infections? They’re not as disastrous as the headlines may suggest (keep reading—more on that below).
Here are some takeaways from our conversations.
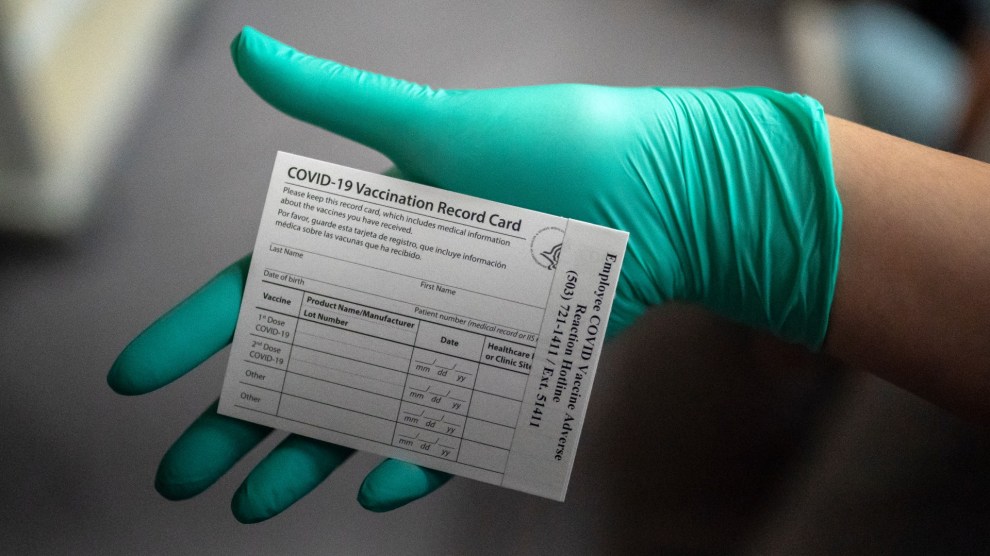
Vaccines are working.
Right now, the CDC estimates the Delta variant makes up about 25 percent of new COVID cases in the US. There are a few places in the country where infections are on the rise, but overall, “most of our hospitalizations across the United States are staying low,” Gandhi says, and continue to decline. “We’re at our lowest number of deaths, luckily, that we’ve ever had.” You can thank the vaccines for that.
So far, data also indicates that breakthrough infections, when they happen, tend to be mild or asymptomatic. In a recent study published in the New England Journal of Medicine, for instance, researchers followed nearly 4,000 frontline workers for four months beginning in late 2020. In that time, 204 workers got COVID, just five of whom were fully vaccinated. (Eleven people who tested positive were partially vaccinated, 156 were unvaccinated, and 32 had unknown vaccination statuses.) And for the few vaccinated workers who got COVID, their infections were less severe than those who were unvaccinated. “It shows that if you have a breakthrough infection after full vaccination or even partial vaccination,” Gandhi says, “that breakthrough infection is really mild.”
For the Delta variant specifically, we’re seeing a similar trend: Vaccines are preventing the worst infections. In the UK, where an estimated 95 percent of infections are with the Delta variant, hospitalizations have also stayed flat—despite a surge in cases. That’s good news, Gandhi says, because it means the vaccine is preventing severe illness. “That actually proves the rule that vaccines work,” she says. Similarly, in Israel, she notes, there have been zero COVID deaths in the last week. And preliminary data from Johnson & Johnson, Pfizer, and Moderna indicate their vaccines do provide protection against the Delta variant.
In the United States, outbreaks caused by the Delta variant are likely to be clustered in areas with low vaccination rates.
As the Delta variant spreads, it’s reasonable to expect that places where people aren’t getting vaccinated will see the worst outbreaks, experts say.
It’s “already starting” in the Ozarks, Hotez says. In southern Missouri, for instance, there is a “perfect storm” of low vaccination rates and a high percentage of the Delta variant. He predicts we’ll see a surge in cases in the South this summer, likely in red states like Louisiana, Mississippi, and Alabama, with adult vaccination rates currently at 45 percent or fewer. “It’ll be of a different character,” he says, “because more of the older adults will be vaccinated. So the deaths won’t be as high. But,” he predicts, “we’ll see a lot of cases and a lot of hospitalizations.” (And, as Hotez points out in a recent article in the Daily Beast, children under the age of 12 are still ineligible for the COVID vaccine. “For that reason,” he writes, “the rise of delta in Ozark and Southern states this summer could make life more complicated for the entire country in regards to school openings in August and other efforts to return to a pre-pandemic normal.”)
Without effective messaging on the right, he says, vaccination rates in conservative areas are likely to remain low. And if the Delta variant reaches those communities, he warns, it could turn ugly. "What's going to happen, basically, [is] anyone at this point who has not been vaccinated, and doesn't plan on getting vaccinated, or has not been infected and recovered, is going to get COVID from Delta variant."
It's unclear if we'll need a booster shot for the Delta variant.
Again, so far, the data we have suggests our vaccines are highly protective against the Delta variant and other variants of concern. If the vaccine is shown to be less effective against this variant, booster shots may be an option to, well, boost our immunity. Pfizer-BioNTech, Moderna, and Johnson & Johnson are currently conducting clinical trials on the benefit of booster shots.
In short, we don't know if booster shots will be recommended.
Another question is, if we do need boosters, will we need variant-specific shots or will another dose of the same vaccine do the trick? That's something scientists are still investigating, Hotez says.
The more transmission there is, the higher the chance that another variant will emerge.
To state the obvious, our best option for combatting the Delta variant is our arsenal of available vaccines. As Gandhi notes, it's "pretty amazing" that "months into mass vaccination, we're still having 750,000 to a million Americans get vaccinated every day."
While there is plenty of reason to be optimistic, experts say we're not out of the woods just yet. "Even if we are fully vaccinated and all our lives are starting to go back to normal," Shafir says, "COVID-19 is still a pandemic." To see our way through this, she says, we need to minimize the chance of transmission "to the greatest extent possible." The fewer cases there are, the less opportunity the virus has to evolve.
As she puts it, "The pandemic isn't over anywhere until the pandemic is over everywhere."