Mother Jones illustration; Ivan Yudin/TASS/Getty
Back in February—a lifetime ago in pandemic time—I spoke with several experts who warned about the United States’ ability to sequence and track coronavirus variants. At the time, scientists in the United Kingdom had identified the pandemic’s first “variant of concern,” a strain later called Alpha. The UK boasted the “gold standard” of genomic surveillance strategies, sequencing about 6 percent of positive COVID samples in early 2021; the US, meanwhile, was sequencing about 0.3 percent. “We’re blind to what’s happening,” one expert in infectious diseases and vaccinology told me.
Alpha would eventually be outperformed in the UK (and the world) by another variant, Delta. But its emergence, among the rise of other variants of concern shortly afterward, was a wake-up call: Without a robust genomic surveillance program, researchers warned, the US would fail to monitor variants as they were introduced or to detect new, homegrown ones—leaving us less prepared to fight the virus.
Enter Omicron. First reported to the World Health Organization by South African officials around Thanksgiving, the variant has since been detected in dozens of countries, including the US. And in much of the news media, the prevailing narrative about the US’s genomic surveillance has remained the same: The country “lags behind” our foreign counterparts, has been “slow to the party,” and is at risk of “flying blind.”
But after talking with a few experts last week, it became clear that this isn’t exactly the case anymore. In fact, the US is far from straggling behind. And in a sea of alarming headlines about Omicron, this is truly good news.
“I feel like the sentiment this time last year was, The US doesn’t sequence enough. We’re behind, we’re behind. And I think it was a fair argument. But at this point, I think it’s just a really lazy argument,” says Joseph Fauver, an assistant professor at the College of Public Health at the University of Nebraska Medical Center, which is working with the state to track variants. “I am unapologetically on the side of, we’re doing an exceptional job. That doesn’t mean we couldn’t be doing things better. But there’s so much data being generated right now across the US and across the world.”
Here, based on my conversations, is what you need to know about Omicron, future variants, and genomic sequencing:
We’ve seen a huge increase in SARS-CoV-2 genome sequencing. Thank federal funding.
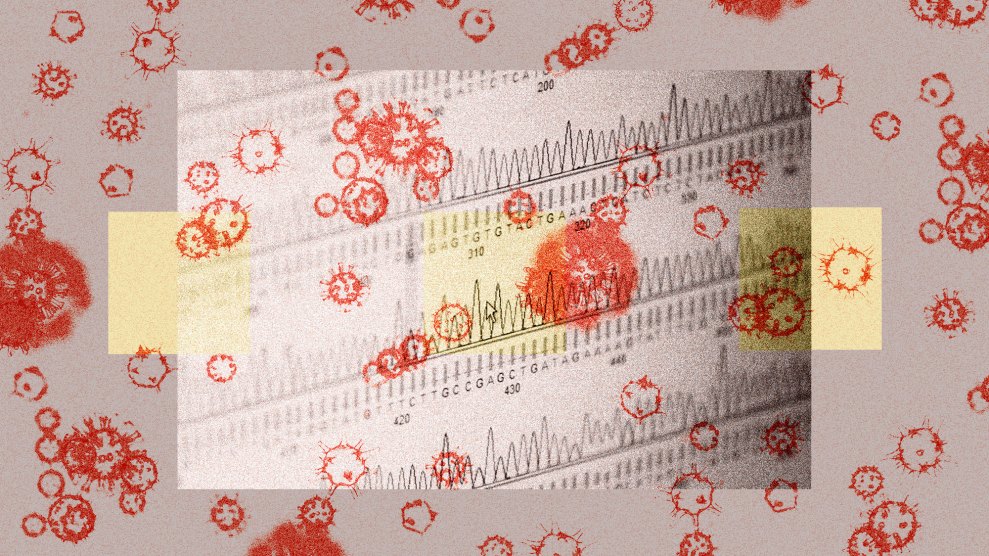
Early this year, when experts called for an investment in the country’s ability to track SARS-CoV-2, the Biden administration listened. In February, it announced a $200 million “down payment” to track variants, followed by a $1.7 billion investment in April. “The CDC, with the support of the White House and federal government, really rolled out a robust plan to get genomic surveillance up to speed across the country,” says Bronwyn MacInnis, director of pathogen genomic surveillance in the Infectious Disease and Microbiome Program at the Broad Institute of MIT and Harvard.
The effort was three-pronged: First, federal health officials worked to get the institutions that were doing large scale COVID testing—shops like Labcorp, Quest Diagnostics, Helix, and the Broad Institute, where MacInnis works—to conduct their own sequencing, giving scientists what she calls a “10,000-foot view” of what strains are circulating across the states.
Second, the administration injected funds into local and state labs, giving them the ability to be “more nimble,” MacInnis says, and zoom in on local outbreaks or perform targeted sequencing in places where it was needed.
The third piece, MacInnis says, was to continue to support academic research centers like hers that are using their lab capacity to track SARS-CoV-2. “It’s not perfect,” MacInnis says about the effort as a whole. “It’s also not easy. But it is really strong.”
The data backs that up: At the start of 2021, the country was sequencing a few thousand genomes per week. In late November, that level hit nearly 100,000 per week. By Fauver’s estimate, the US has sequenced about as many, if not more, SARS-CoV-2 genomes as we have for all other viruses combined.
“At the beginning of this year, we still weren’t sequencing enough to really get a good snapshot of what was circulating in the US,” adds Alexandra Phelan, an assistant professor at the Center for Global Health Science and Security at Georgetown University, whose work focuses on pandemic preparedness and response. “If we look at us now, we are actually in a much, much better position.”
As a result, we have a much clearer view of what variants are circulating here.
In addition to sequencing tens of thousands of samples per week, we're also hitting our goal in terms of percent of cases sequenced. In early 2021, scientists had set a goal of sequencing five out of every 100 positive COVID samples. According to a preliminary but widely cited analysis by Illumina, a San Diego–based company that makes genomic sequencing equipment, the US would need to sequence 5 percent of samples to detect a variant that makes up between 0.1 percent and 1.0 percent of cases.
As of now, on average, we're there: "I would say most states are now at or close to that five percent mark," MacInnis says, "and many are well beyond it." (Last week, CDC Director Rochelle Walensky told reporters the agency is sequencing at a rate of about one in seven positive samples, or about 14 percent.)
Five percent may not sound like a lot, but testing well beyond that has "diminishing returns," MacInnis says. "It's unrealistic at this point to sequence every positive case. And it's also kind of unnecessary." With a rate of 5 percent, "we have the power to detect emerging threats at an early stage." If a new variant is going to result in "any meaningful number of cases," Fauver adds, "we will absolutely detect it with that level of sequencing."
As cases rise, genomic sequencing gets harder.
One way to make researchers' jobs easier? Lowering the total number of COVID cases. Think of it this way: The rate of genomic sequencing is the number of SARS-CoV-2 sequences divided by the number of positive tests in the US at a given time. If we want to increase our rate, we can either increase the number of genomes sequenced or lower the number of cases. “There's effectively unchecked COVID transmission occurring right now,” Fauver says, “making it really difficult to raise that percentage.”
This is also partly why countries like Iceland or New Zealand are able to sequence a huge percentage of positive samples: low case counts. The US may rank 22nd in the world for our percentage of sequenced genomes, but we're also dealing with a lot of cases. "The absolute value of that number really matters," Fauver says. "I think it's really easy to sequence 100 percent of cases occurring in a week if you only have 1,000 cases."
Plus, Fauver points out, lowering case counts also reduces the chances of new variants being introduced in the population in the first place. "If you're not infected," he says, "you're not going to be a part of generating a new variant."
We still have some "blind spots" around the country.
While the US is sequencing at a rate of 5 percent, that number, experts emphasize, is an average. Some states aren't sequencing nearly as many genomes as others. Oklahoma, Phelan notes, has sequenced less than 1 percent of all its samples over the pandemic. By contrast, Washington, which was among the first states to be impacted by the coronavirus and is home to several academic institutions, has sequenced at a rate of about 8 percent since January 2020. In Wyoming, it's 20 percent. In Vermont, it's 22 percent.
Those disparities exist, Fauver says, in part because of what kinds of institutions exist in each state. Take California. The state has published nearly 300,000 sequences since the start of the pandemic, more than any other state. Yes, it's a big population—"but," Fauver says, "think of all the groups in California that are producing whole-genome sequencing data." County labs, state labs, institutions like the Scripps Research Institute and UCSF, nonprofits like the Chan Zuckerberg Biohub, and private companies like Illumina all operate in the state. "All that is going to push California's numbers up a lot," he concludes. In Nebraska, where Fauver is based, researchers have been able to generate "really high-quality data routinely," he says, but the effort is primarily being run by the state, in combination with a small handful of academic partners.
On top of state disparities, experts are concerned that the states that aren't sequencing as many samples are often the states with lower vaccination rates. That is, states where new variants are most likely to emerge are also the places that aren't looking as closely. "There is a risk that there is undetected spread," Phelan says.
In a 2020 report, Phelan and others called on the federal government to establish a unified approach to genomic data sharing. We still need it, she says: "A lot of this data is fragmented because the country and the health systems are fragmented. We still need a comprehensive and systematic sharing across the country between states and at the federal level."
Travel bans and other measures may disincentivize sharing of genomic data.
Shortly after South Africa reported Omicron to the WHO on November 26, the US instituted travel bans against it and seven other countries, all in Africa. Since then, the Omicron variant has been detected in many other countries, including Canada, the UK, Australia, and Germany, and dozens of others, but the US hasn’t issued any new travel bans against them.
While travel bans may slow the global spread of a variant in early stages—"It's just a basic matter of mathematics,” Phelan says—they are unlikely to stop a variant in its tracks. For one, they can give governments a false sense of security, Phelan says, and are often “inappropriately targeted" to protect public health. In the case of Omicron, for example, "It's hard to not see that as deeply discriminatory."
Experts also worry these restrictions may discourage other countries from publishing their COVID data in the future. “If [sharing information] is met with travel restrictions, I don't see the incentive for these folks to share their data,” Fauver says. “So yeah, I think it sends the exact wrong message.”
And "not only does it disincentivize reporting about variants, but this will impact future outbreaks," Phelan says. If imposing discriminatory travel bans becomes the norm, she adds, "I do worry that we're much less prepared for the next pandemic."
This piece has been updated.