Angela Weiss/Getty
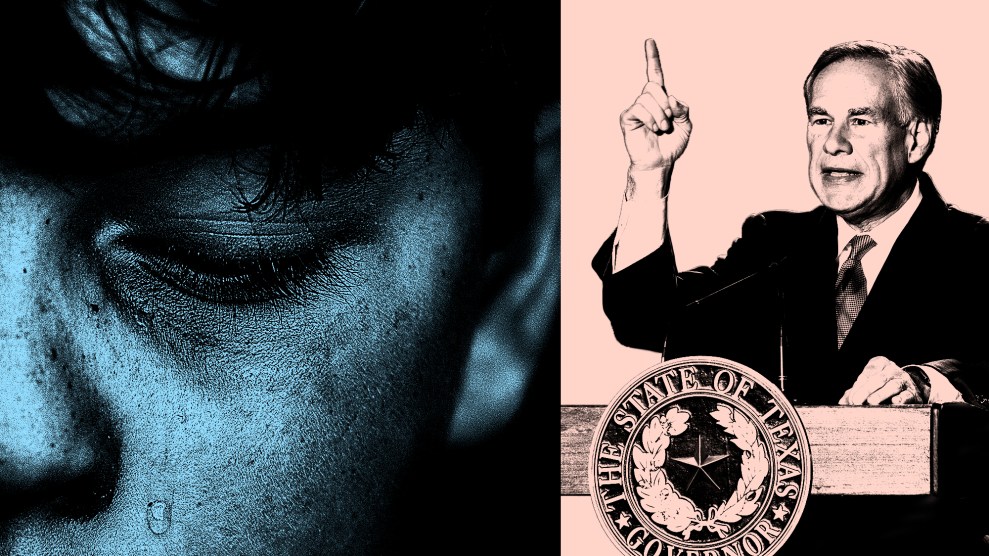
Shauntae Anderson lived for the weekends. Growing up Black and transgender in a small West Virginia city in the 1990s, she spent a lot of time alone, hiding her self-knowledge from her mom and coping with ridicule from classmates. Yet on Friday and Saturday nights, she could lock herself in her room, put on Whitney Houston or Aretha Franklin, and try on the few pieces of women’s clothing she’d stashed away. “I would put those things on, put makeup on, and look at myself in the mirror. Make myself so I felt pretty,” Anderson, now 46, says. Yet the night always had to end. “Silent tears would just flow down my face as I’m wiping it off,” she remembers.
When she came out to her doctor as a teen, Anderson says she was told there was nothing they could do for her. As an adult without health insurance, she wanted her body to change so badly that she tried popping birth control pills for their minuscule dose of hormones. It wasn’t until she was 40 years old and incarcerated in a federal prison that a doctor finally agreed to treat her gender dysphoria, the medical diagnosis for what she’d been going through.
Finally getting the prescription hormones she’d needed for so many years was “liberating,” Anderson says. Her skin softened; her breasts grew. Her cellmate, also trans, pointed out gradual changes in her figure.
But when Anderson was released from a halfway house in 2020, she ran into what she calls a “brick wall”: Medicaid. Under West Virginia policy, Medicaid would cover her hormones but not the surgeries she needed to continue her medical gender transition. To foot the bill herself was “completely impossible,” Anderson says. She already struggled to cover bills, working two minimum-wage jobs with zero credit after prison. Her transition ground to a halt, and her gender dysphoria began to worsen. “I got to a point where it got hopeless,” she says. “Because I was back to square one.”
In late 2021, Anderson agreed to join a lawsuit challenging West Virginia’s Medicaid exclusion for gender-confirming surgery. The case, filed by the LGBTQ civil rights organization Lambda Legal and local partners, argued that West Virginia was violating federal anti-discrimination law by denying coverage for surgical procedures used to treat gender dysphoria, while approving them for other diagnoses.
Last August, they won: A federal judge threw out West Virginia’s Medicaid exclusion. “The same or similar surgical treatments are available…when the diagnosis requiring that treatment is not gender dysphoria,” District Court Judge Robert Chambers wrote in his ruling, pointing to mastectomies as an example. “When treatment is precluded for a diagnosis based on one’s gender identity, such exclusion invidiously discriminates on the basis of sex and transgender status.”
The victory in West Virginia owes a lot to a landmark 2020 Supreme Court decision, which ruled that the federal civil rights law banning sex discrimination in employment extends to trans and gay workers. In 2021, Alaska agreed to eliminate its exception to settle a lawsuit by a woman, Swan Being, who was denied coverage for costs related to her hormone treatment. Georgia followed suit in a similar settlement last July, agreeing to drop its exception for gender-confirming surgery. And a case challenging Florida’s Medicaid exclusion is headed to trial in May. Carl Charles, an attorney at Lambda Legal who worked on the other Medicaid cases, filed the Florida lawsuit on behalf of trans Medicaid recipients and their families last fall after Gov. Ron DeSantis’ Agency for Health Care Administration rammed through new regulations cutting off coverage for puberty blockers, hormones, and surgeries.
The momentum to guarantee Medicaid coverage for transgender medical care is a ray of light at a time when trans rights are under sustained attack from Republican state legislators, who are pushing bills across the country to restrict gender-affirming care. The targeted medical treatments—which typically include puberty blockers for pubescent children, cross-sex hormones for teenagers or adults, and, almost exclusively for adults, surgeries—are supported by the major medical associations and widely considered lifesaving. Yet as of January 30, 21 states are considering 77 bills to restrict LGBTQ health care, according to the ACLU. On Saturday, Utah Gov. Spencer Cox signed a bill banning gender-affirming surgery for people under 18 and putting a “moratorium” on puberty blockers and hormone treatments for minors newly diagnosed with gender dysphoria. Two more states, Alabama and Arkansas, have already prohibited gender-affirming treatments for youth, though both bans are currently on hold thanks to court challenges. (Arizona and Tennessee have also banned some gender-affirming care for minors with gender dysphoria, but their laws have little practical effect, according to trans rights legal experts.)
Even as these battles play out, gender-affirming care is already effectively banned for tens of thousands of trans adults and an unknown number of children who, like Anderson, get their health insurance through Medicaid. Nine states maintain Medicaid policies that explicitly exclude coverage for gender-affirming medical treatments such as surgery, hormones, and therapy, according to an analysis of state Medicaid polices by the Movement Advancement Project. As a result, full gender-affirming care is out of reach for over 50,000 trans adults who are low-income or have a disability, according to population estimates from the Williams Institute.
Half of those Medicaid recipients live in states like Tennessee and Texas that chose not to expand Medicaid eligibility—meaning the people impacted fall below an extremely low income threshold. “It would be basically impossible for those folks to afford gender-affirming care out of their own pocket,” Charles says. “They are really working with incredibly limited resources.”
Medicaid coverage is especially vital to trans people’s access to health care as whole. In a 2015 survey of trans people’s experiences, 29 percent of respondents lived at or near the poverty line—more than twice the rate of the US population—and, in 2014, about 1 in 8 had an income of less than $10,000. That’s the result of systemic discrimination, harassment, and violence, which often begins at home, continues throughout their education, and follows trans people into the workplace. Many are “struggling to hold down a job because cisgender people would not allow it,” Charles explains. “Whether it’s making access to the bathroom impossible, not letting people present as their accurate gender, or straight up firing them when they come out.” As of summer 2021, those who managed to remain in the traditional workforce were making 30 to 40 percent less on average than the US median weekly salary of $1001, according to a poll by the Human Rights Campaign.
“Any place where there’s an exclusion on the books, you also have to think about transgender Medicaid participants who oftentimes don’t have the resources or means to access this vital care on their own,” says Avatara Smith-Carrington, a Lambda Legal attorney working with Charles to challenge state Medicaid exclusions for transgender health care. “Because that could mean not having money for rent, not having money for food, not having money for all the other things that people need just to survive and thrive day to day.”
Yet Medicaid exceptions have been a reality for years in places like Arizona, which has blocked coverage for gender-confirming surgery since at least 2004. Others Medicaid bans, like Florida’s, are brand new. At least two states, Oklahoma and Virginia, are currently considering proposals similar to Florida’s, as part of larger bills that would punish doctors for providing gender-affirming care to people under 21. Fifteen more states have Medicaid policies that are silent or unclear about whether gender-affirming care is covered, leaving another 50,000 adults in limbo. “I do think there is a cause for concern, particularly when we’re looking at the states that don’t have explicit policies in support,” Charles says. “Republican conservative state senators are thinking, ‘Hmm, we should take a look at our Medicaid program.'”
According to Charles, the legal wins against the Medicaid exclusions help exert pressure on private insurers deciding whether to cover transgender health care. They may also bode well for pending court challenges to other gender-affirming care restrictions. Utah is expected to face a lawsuit over its new ban shortly.
Meanwhile, in West Virginia, the state government is appealing the ruling that eliminated the Medicaid exclusion for gender-confirming surgery. But for now, the lower court’s decision stands. On the day that we talked, Anderson was looking forward to an appointment to discuss a potential procedure. “I’m really excited,” she tells me. “It’s like another chapter in this book of mine.”