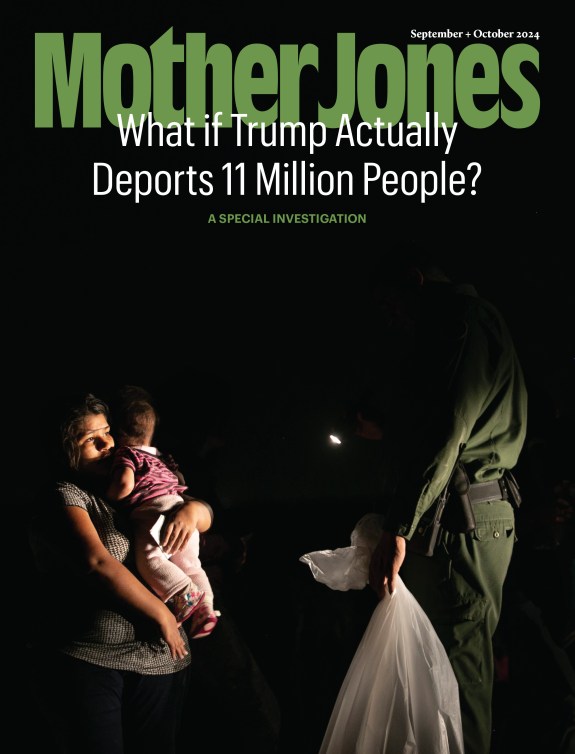
Gosia Wozniacka/AP
This story was originally published by Inside Climate News and is reproduced here as part of the Climate Desk collaboration.
For most of July 2019, stifling heat hung over the agricultural fields of California’s Central Valley, as farmworkers like William Salas Jiminez labored under the sun’s searing rays. Temperatures had dipped from 99 to 95 degrees Fahrenheit the last day of the month, when the 56-year-old Puerto Rico native was installing irrigation tubing in an almond orchard near Arvin, at the valley’s southern edge.
Around 1:30 that afternoon, Salas sat down to rest. When he stood up to go back to work, he suddenly collapsed. An hour and a half later, he was dead. Reports filed with the US Department of Occupational Health and Safety, or OSHA, say Salas died of a heart attack.
Salas’ death certificate lists atherosclerotic heart disease as the immediate cause of death. But it also lists “extreme heat exposure” and obesity as significant contributors. Both heart disease and obesity increase the risk of fatal heatstroke.
No federal standard protects workers from extreme heat, though OSHA proposed a rule in 2021—a half-century after public health officials first recommended precautionary measures. California was the first of the five states that have passed a heat exposure standard and its requirements are considered among the toughest. Yet the standard doesn’t recognize an increasingly dangerous threat for agricultural laborers in a warming world: working in hot, polluted air.
According to the 2022 annual report from California OSHA, or Cal/OSHA, just two California farmworkers died from heat exposure between 2018 and 2022.
But an Inside Climate News review of federal farmworker death records, along with temperature and air pollution data, suggests the numbers may be much higher. Scores of farmworkers died in California between 2018 and 2022 when temperatures exceeded the threshold that triggers California’s heat safety requirements. All of these deaths occurred in counties with chronically unsafe air.
Eighty-three of the 168 farmworkers who died suddenly at work in California from 2018 to 2022 perished when temperatures exceeded 80 degrees Fahrenheit—when employers must provide adequate fresh water, shade, and rest to cool down—within a day of their death. Thirty-six of these 83 workers died of heart attacks, strokes, or other cardiovascular diseases; unspecified underlying medical conditions; or unknown or “natural causes.” Twelve died of respiratory conditions, including COVID-19, and one died of methamphetamine toxicity. The other 34 died from injuries sustained in accidents. Heat stress is known to increase the risk of death from cardiovascular and respiratory conditions, including COVID-19, drug use, and workplace accidents.
In three of these cases, air quality for hazardous tiny particles called PM2.5 within a day of a worker’s death was also “unhealthy for sensitive groups,” when people with underlying heart or lung conditions should minimize long or intense outdoor activities. But even if the air quality was normal on the days workers died in the heat, every county they worked in received a failing grade for short-term particle pollution in the American Lung Association’s State of the Air report.
Scientists are gaining new insights into the complex constellation of factors that interact with heat to cause illness and death. They know workers can die of heat stroke even when temperatures fall below the low 80s. They know existing reporting measures vastly underestimate heat-related injuries and deaths. And they’ve discovered that simultaneous short-term exposure to heat and fine particle pollution, both deadly on their own, may be particularly lethal.
It would take a rigorous study to determine whether heat or air pollution triggered the deaths Inside Climate News identified, but it is clear that California’s farmworkers are at high risk, said Paul English, an environmental epidemiologist and director of the Public Health Institute’s Tracking California, a project aimed at improving public health.
The scientific literature shows that conditions of high heat stress the heart, English said. “And there’s been more and more research about air pollution and small particle pollution being related to heart attacks and to hospitalizations and emergency room visits for heart attacks.”
The incidence of fatal heart attacks, strokes, and other cardiovascular events linked to high temperatures increased sevenfold globally between 1990 and 2019, researchers reported in the European Journal of Preventive Cardiology in October. Exposure to high levels of fine-particle pollution over just a few hours can trigger cardiovascular-related deaths.
Fine particles can interact with high heat to double the risk of fatal heart attacks when compared with either exposure in isolation, a recent study in China published in the journal Circulation found. It’s unclear how well the results apply to other geographic regions, the researchers cautioned. But the study corroborates previous evidence that co-exposure heightens the risk of death. And the San Joaquin Valley, where three-quarters of the deaths occurred, has the worst PM2.5 pollution in the nation.
“It’s difficult to say which aspect of an exposure specifically led to someone’s heart attack or stroke,” said Sameed Khatana, a cardiologist and researcher at the University of Pennsylvania Perelman School of Medicine. But it’s clear from population-level data that when extreme heat or bad air days occur, he said, “more people seem to die from heart attacks and other causes as well.”
When asked if Cal/OSHA will revise its standards in light of new evidence that simultaneous exposure to heat and PM2.5 doubles death rates, a spokesperson for the Department of Industrial Relations, which houses Cal/OSHA, did not address the question but said the agency continues to enforce its rules for heat illness prevention and protection from wildfire smoke, which emits PM2.5.
For Daniel Smith, an assistant professor at Villanova University’s College of Nursing, working out whether heat played a role in a specific person’s death is a classic chicken or egg question.
“If a worker hadn’t been working in the heat,” Smith said, “they likely would have never died from the myocardial infarction, the renal failure, the dehydration, the heat stroke.”
The San Joaquin Valley is the most productive agricultural region in the world. But rising temperatures and chronic air pollution make it an increasingly dangerous place to work.
In just over four weeks during the month in 2019 when Salas died, five other farmworkers died abruptly when temperatures were between 85 and 95 degrees in counties with notoriously bad air quality.
At 6 a.m. on July 18, a 63-year-old man climbed onto a tractor to spray fields with pesticides, then parked his rig alongside a cornfield in the early afternoon. When he failed to come home after his shift ended, his worried relatives went looking for him. It was still in the low 90s after 8 p.m., when they found his body in the cornfield. No cause of death was given. Three days earlier, a 50-year-old man was chopping weeds before lunch in a raisin vineyard when he started feeling sick and sat down to rest. Minutes later his supervisor saw him facedown under the vines. OSHA records say he died of cardiac arrest. On the afternoon of July 5, a teenager had been driving a tractor when it ran over and killed him three weeks before his 19th birthday. No one knows how he got off the tractor. Just two weeks earlier, a young woman had taken ill while working in a vineyard and fell into a coma after convulsing on the way to the hospital. The 20-year-old died at the hospital of an aneurysm, investigators said. Less than 24 hours earlier, a 30-year-old man stopped pruning pistachio trees to drink water and rest in his truck, where he died. Heart attack, OSHA records say.
“Sadly, it is not surprising to hear about so many farmworker deaths that are likely related to the conditions they face in the workplace, including exposure to excessive heat and air pollution,” said Mayra Reiter, project director of Occupational Safety and Health for the nonprofit Farmworker Justice.
Farm work is already one of the most dangerous occupations, advocates like Reiter say, and now climate change is making it even riskier.
The valley is likely to see a sevenfold increase in extreme heat days, California’s Fourth Climate Change Assessment predicts. Its counties repeatedly fail to meet federal particle pollution standards.
PM2.5, a mixture of fine particles too small to see with a conventional microscope, results from burning fossil fuels in vehicles, factories, and power plants and burning wood in homes, agricultural emissions, and wildfires, among other sources.

Fine particles can linger in air for weeks, lodge deep in the lungs, enter the bloodstream, and damage nearly every organ in the body, including the brain, increasing the risk of deadly coronary and cerebrovascular events.
“When it comes to particulate matter, there’s growing evidence that there is probably no safe level,” said Khatana of the University of Pennsylvania.
Heat forces the body to work harder to keep its internal temperature in check, straining the lungs, heart, and kidneys. The heart pumps harder and faster as blood vessels dilate and blood pressure drops, reducing blood flow and oxygen to the brain and increasing the risk of fatal heart attack and respiratory distress.
Heat-triggered damage to the lungs and heart, combined with preexisting cardiovascular and respiratory diseases and elevated air pollution, are the leading causes of death during heat waves, researchers reported in a 2021 review of heat and health risks in The Lancet.
Researchers are just starting to get a handle on the prevalence of these conditions among farmworkers. More than a third of California farmworkers rated their health as fair or poor in a University of California, Merced Community and Labor Center survey published in February. The survey supports earlier research showing a higher prevalence of chronic diseases among farmworkers that increases their vulnerability to heat, including elevated blood pressure and cholesterol, diabetes, obesity and asthma.
Villanova’s Smith called it imperative to recognize the danger heat poses for people with a preexisting condition. “Workers should be able to work and earn a living in an environment that is safe enough for them to work, even if they have an underlying arrhythmia.”
The California Farm Bureau did not respond to a request to comment, but encourages growers to have systems in place to contact emergency workers to respond to heat-stress cases.
Heat can also boost pesticide vaporization, leading to higher application rates and increased exposure to agrochemicals.
Adding to their risks, workers who fuel the region’s $37 billion agricultural market earn so little—an average annual wage of $21,915 in 2019, according to a UC Merced Labor Center study—they often keep working when heat and unhealthy air conspire to threaten their lives.
“It’s very easy to forget that there are people behind the food you eat every day,” said Kristina Dahl, a climate scientist with the Union of Concerned Scientists. “We have to find ways to protect these workers, but also find more humanity in ourselves to recognize and not accept the cost that is associated with our food.”
Death from heat stroke among outdoor workers has risen over the past two decades along with temperatures driven higher and higher by the burning of fossil fuels. Agricultural workers face more than 35 times the risk of heat-related deaths than other occupations, a 2016 analysis of federal labor statistics found.
The Bureau of Labor Statistics, which records worker heat-related fatalities, injuries, and illnesses, has been counting about 40 fatalities per year in recent years, Rosemary Sokas, a physician and occupational health expert at Georgetown University, told the New England Journal of Medicine in a podcast in October. “But that’s the tip of the iceberg.”
For one thing, bureau statistics exclude farms with fewer than 11 employees and don’t account for the part-time nature of most farm jobs. Plus, the number of “slips, trips and falls,” which cause some 700 deaths a year across occupations, aren’t included in the bureau’s heat fatality statistics, Sokas explained. Neither are fatal injuries or accidents that happened when workers were overheated.
Yet accidents on the job rise with temperature, as people grow increasingly weak, fatigued, uncoordinated and disoriented. Heat stress impairs cognitive function, concentration and reaction time, studies show, leading to fatal injuries and accidents like falling from a ladder while harvesting fruit.

The Bureau of Labor Statistics may be missing thousands of heat-related illnesses across occupations, an analysis of nearly two decades of workers’ compensation claims found. Up to six times as many of the claims were filed for (both indoor and outdoor) heat-related illness in California than the bureau’s records captured.
Preliminary results of a similar review of California workers’ comp claims found that high temperatures resulted in roughly 20,000 additional injuries a year, including injuries seemingly unrelated to temperature like severing a limb in machinery or getting run over by a vehicle,
The evidence suggests that the true number of heat-related illnesses may be 10 times higher than the official record, Jisung Park, a public policy researcher at UCLA who led the study, said in September during a meeting of a new state-mandated heat advisory committee. “It isn’t just heat illnesses we should be worried about,” Park said, “but also a much wider range of ostensibly unrelated accidents that are nevertheless increased due to hotter temperatures.”
More than three-quarters of the accidents that killed California farmworkers between 2018 and 2022 involved fatal encounters with tractors, farm machinery, or toxic chemicals.
“Federal OSHA officials have been making the case all through the rulemaking, which has been going on for two years now, that the data available are underestimates,” said Juanita Constible, senior advocate for climate and health at the Natural Resources Defense Council, or NRDC.
The lack of reliable data stems partly from a lack of reporting by employers and by workers who fear they’ll lose their job or, if they’re undocumented, get deported, Constible found in an NRDC report published last year. Although undocumented California workers are eligible for workers’ comp, many are wary of filing a claim they fear could be used against them or lack the literacy to fill out the paperwork.

Because there are no standard criteria for classifying heat-related deaths, medical examiners may list the cause of death as a heart attack or similar condition when the actual or aggravating cause may have been heat-related, an OSHA memo outlining efforts to reduce heat-related incidents said.
The Centers for Disease Control and Prevention relies on death records to estimate that about 700 people die from heat exposure in the United States a year. But when researchers look beyond what’s recorded on a death certificate, they see a much greater incidence of deaths associated with heat, said the University of Pennsylvania’s Khatana.
“Papers like ours suggest that the number of deaths could be as high as 2,000 or more a year,” Khatana said, referring to a study of excess deaths associated with extreme heat among U.S. adults published last year in JAMA Open Network. “Other studies have suggested even higher levels.”
Khatana and his colleagues went on to show that heat triggered heart attacks and strokes in half of those deaths.
Farmworkers are particularly vulnerable to heat-related fatalities because their pay often depends on how much they harvest.
Yet California’s standard doesn’t outline the steps employers should take to ensure workers adjust to the heat or how close water and shade should be, said NRDC’s Constible. “For farmworkers, that’s a particular problem because they’re working in big fields and often have to walk quickly on a very short break to try and get some water and then go back to where they were working.”
What’s more, about a third of farmworkers speak Indigenous languages like Mixteco or Triqui and are not fluent in English or Spanish. They’re less likely to receive training about heat in their language or to complain when their employer doesn’t provide adequate breaks, shade or water.
That means workers may not recognize a rapid heartbeat, heavy sweating or headaches as a sign of dangerous heat stress, advocates say.
Cal/OSHA inspectors are tasked with making sure employers implement heat-illness training and prevention plans. Yet the agency has just 14 inspection officers for the entire state who speak Spanish and none who speak an Indigenous language, according to Garrett Brown, a former Cal/OSHA investigator who retired in 2014 and tracks what he calls the agency’s decline.
State offices are severely understaffed, with more than 100 field enforcement positions unfilled as of October, Brown said. Even if all the vacancies were filled, Cal/OSHA would have just one inspector for every 110,000 workers, a ratio Brown called “ridiculous.”
Some of the district offices have a 60 percent vacancy, Brown said. “That means there’s no enforcement there at all.”
Cal/OSHA is “diligently” hiring health and safety staff to conduct inspections across the state, a Department of Industrial Relations spokesperson said, noting that it is challenging to recruit and retain qualified experts.
Even when there is enforcement, small financial penalties, and weak criminal sanctions fail to deter employers who cut corners and endanger workers, two former top OSHA administrators argued in a 2020 analysis published in the American Journal of Public Health.
Of more than 1,000 heat citations issued to agricultural employers in California since 2018, penalties were reduced in nearly half of the cases for an average fine of $2,625, an Inside Climate News review of Cal/OSHA citations found. More than 215 employers had at least two violations.
“The penalties and level of enforcement just aren’t enough to keep workers safe,” said Constible, who reviewed OSHA citations and penalties against employers who violated California’s heat standard for the NRDC report.
Monetary penalties are determined by regulations and employers have the right to contest any citation or penalty, a Department of Industrial Relations spokesperson said. Ultimately, the spokesperson added, “employers bear the responsibility to maintain a workplace free of safety and health hazards.”
Yet as Constible sees it, Cal/OSHA is not sufficiently addressing the pattern of “using and abusing workers.” Although it’s a problem all across the country, she said, “I expect better from California.”
Cal/OSHA clearly needs to increase its inspections to make sure that employers are complying with California’s heat standard and workers are getting the protections they are entitled to, said Reiter, of the Union of Concerned Scientists.
“What is happening in California is probably happening in states with no heat regulations, underscoring the urgent need for a federal standard,” Reiter said. “Farmworkers should not have to die in order for us to eat.”